Laboratory values
Understanding holistic laboratory analyses - What your results reveal.
Lab results are key to a deeper understanding of your health. A holistic lab analysis doesn't view the body in isolation, but as an interconnected system of metabolism, hormones, nutrients, and immune defense. This allows imbalances to be detected early – even before symptoms develop.
Understanding your lab results empowers you to actively manage your health. Holistic analyses provide clarity and guidance for a sustainable balance of body, mind, and metabolism.
Whole blood mineral analysis (capillary):
It measures minerals and trace elements directly in the cells and in the plasma, i.e., in the entire bloodstream – not just in the serum. This allows it to better reflect the actual cell status and metabolic state. Particularly for magnesium, zinc, selenium, and iron, it provides more meaningful values regarding tissue supply. Furthermore, a capillary fingertip sample is sufficient, making the method quick, gentle, and practical.
selenium
Selenium in whole blood.
Meaning:
Selenium is an essential trace element that the body cannot produce itself and therefore must obtain through food.
It plays a central role as a component of various selenoproteins, including in particular glutathione peroxidase (GPx) – an important antioxidant enzyme that prevents cell damage caused by free radicals.
Furthermore, selenium is important for:
- Thyroid function: Component of the deiodinases that convert T4 (thyroxine) into the active T3 (triiodothyronine).
- Immune system: Supports the activity of T cells and protects immune cells from oxidative stress.
- Anti-inflammatory properties and possible cancer-protective effects (in physiological amounts).
- Detoxification Glutathione peroxidase (GPx)
Interpretation:
Reference: 100–140 µg/l. Optimal range (preventive medicine): 140–160 µg/l (maximum enzyme activity).
Selenium in whole blood – meaning and interpretation
Possible causes of low selenium levels
- Low intake through diet: Central European soils are low in selenium, therefore grains and plant-based foods often contain little selenium.
- Vegetarian or vegan diet: Animal products (especially fish, meat, eggs) are the main sources.
- Increased consumption: In cases of inflammation, infections, oxidative stress, or chronic diseases.
- Malabsorption: For example, in cases of chronic inflammatory bowel diseases, celiac disease, or after gastrointestinal surgery.
Additional diagnostics
- Glutathione peroxidase (GPx): Activity measurement allows conclusions to be drawn about functional selenium status and detoxification capacity.
- Thyroid parameters: TSH, fT3, fT4 – for assessing thyroid function.
- Selenium levels in whole blood: Control measurement after 3–6 months of substitution or dietary changes.
- CRP / Inflammatory marker: Used to assess whether low levels could be caused by acute or chronic inflammation.
zinc
- Title: Zinc in whole blood.
- Significance: Cofactor of numerous enzymes, important for the immune system, skin, hormone and cell function.
Interpretation:
- (Reference: 7.0–7.6 mg/l) → within the optimal range.
Additional diagnostics: In cases of inflammation, evaluate CRP levels, as zinc can decrease during acute phase reactions.
copper
Designation: Copper in whole blood.
Importance: Component of enzymes involved in iron utilization, antioxidant defense, and collagen synthesis.
Interpretation:
Its value: 1.01 mg/l (reference: 0.85–1.05 mg/l) → normal.
Additional diagnostic testing: Ceruloplasmin in cases of suspected storage diseases or inflammation.
magnesium
Title: Magnesium in whole blood.
Importance: Cofactor of many enzymes, important for muscles, nerves, and energy production.
Interpretation:
Its value: 36.1 mg/l (reference: 35.0–39.0 mg/l) → optimal.
Additional diagnostic testing: Not routinely required.
Calcium
Title: Calcium in whole blood.
Importance: Bone substance, involved in muscle contraction, blood clotting and cell metabolism.
Interpretation:
Its value: 65.6 mg/l (reference: 57.0–61.0 mg/l) → elevated.
Possible causes: Vitamin D supplementation, increased bone resorption, hyperparathyroidism.
Additional diagnostic tests: Serum calcium (ionized), parathyroid hormone, 25(OH) vitamin D, kidney function.
potassium
Title: Potassium in whole blood.
Importance: Important for muscle contraction, heart rhythm and cell function.
Interpretation:
Its value: 1792 mg/l (reference: 1750–1900 mg/l) → within the normal range.
Additional diagnostic testing: Only in case of clinical suspicion (e.g., cardiac arrhythmias).
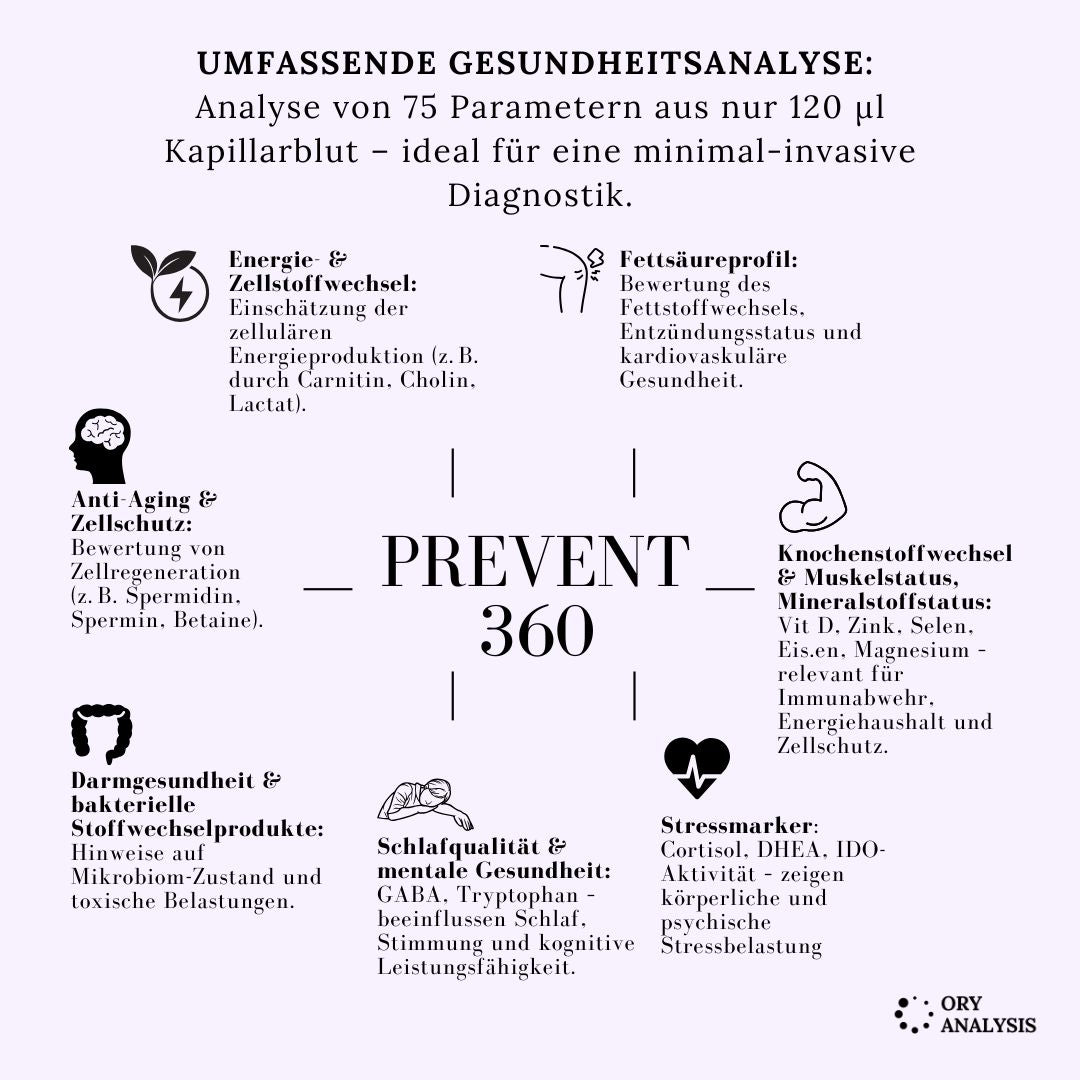
Prevent 360 – Holistic health and metabolism check
The Prevent 360 test is a comprehensive laboratory diagnostic test that holistically analyzes metabolism, micronutrient supply, energy production, detoxification performance, the intestinal microbiome and fatty acid balance.
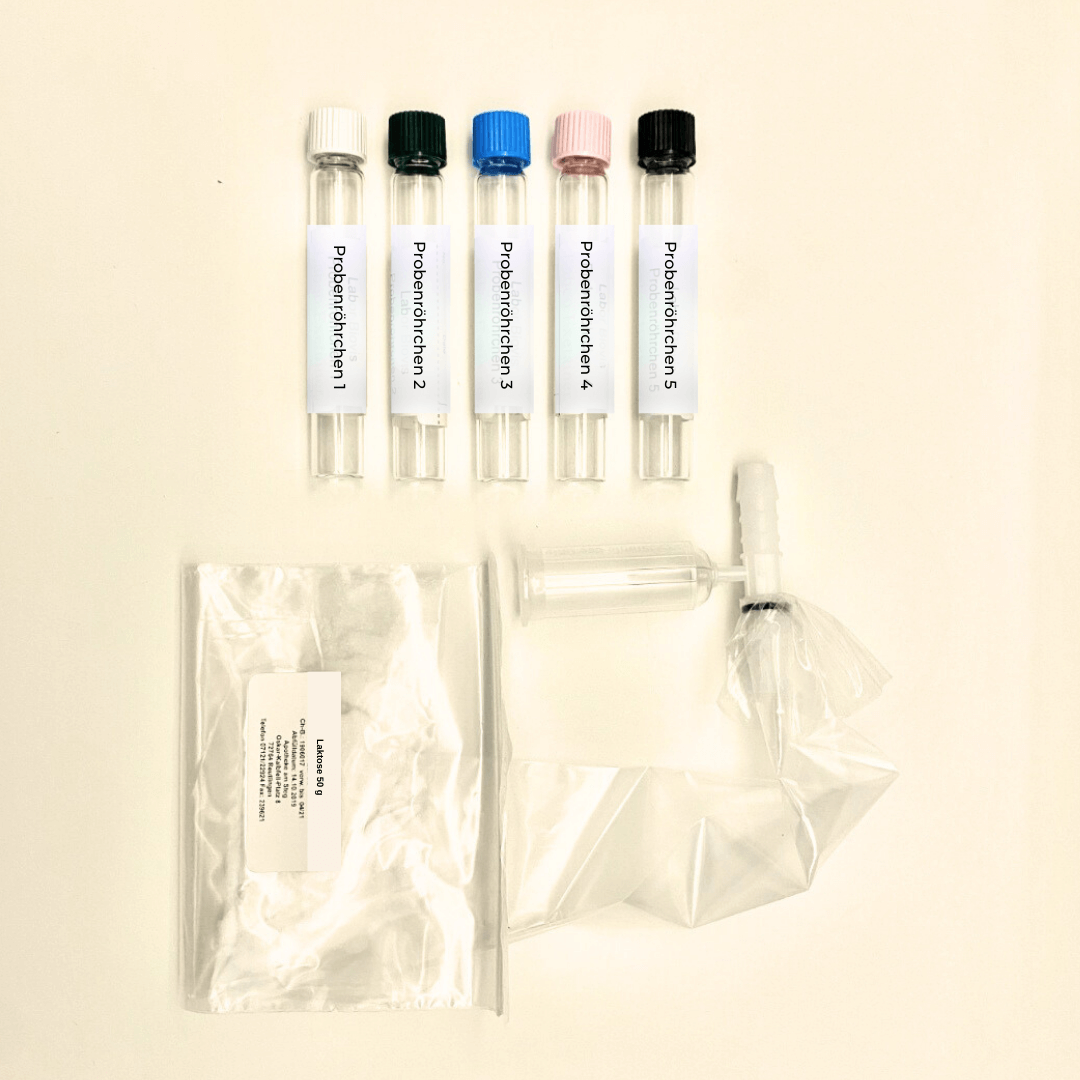
It is based on a capillary blood sample (MITRA) and covers over 60 laboratory parameters – from vitamins and minerals to amino acids, bile acids and stress hormones.
Vitamin D3 (25-OH-Vitamin D)
Laboratory diagnostic name: 25-Hydroxy-Vitamin D3 (Calcidiol).
Meaning / Description: Fat-soluble vitamin, important for bone metabolism, immune system, muscle function and mood.
Interpretation:
Its value: 15 ng/ml (< 30 ng/ml) → Vitamin D insufficiency / deficiency.
Possible consequences: reduced immune system, muscle weakness, low mood, risk of osteopenia.
Additional diagnostics: 25(OH)D check after 3 months of therapy; if necessary, calcium, magnesium, PTH; combination with vitamin K2 is advisable.
magnesium
Title: Magnesium in capillary blood.
Importance: Cofactor in > 300 enzyme reactions (energy production, muscles, nerves, heart rhythm).
Interpretation: 36.8 mg/l (reference 34–39.5 mg/l) → lower normal range / tending towards low.
Additional diagnostics: Whole blood magnesium levels, if necessary magnesium/potassium balance; in case of muscle cramps, consider IV or oral substitution.
zinc
Name: Zinc in capillary blood.
Importance: Immune defense, skin, wound healing, antioxidant protection.
Interpretation: 7.25 mg/l (norm 6.7–7.7) → optimal.
Additional diagnostic testing: None required.
selenium
Name: Selenium in capillary blood.
Significance: Component of glutathione peroxidase (antioxidant, thyroid, immunity).
Interpretation: 50 µg/l (reference 96–130 µg/l) → significantly reduced.
≥ 120 µg/l would be optimal as a preventive measure.
Additional diagnostics: GPx activity, thyroid parameters; whole blood selenium check after 3 months of supplementation.
iron
Name: Iron in capillary blood.
Significance: Component of hemoglobin and cellular respiration.
Interpretation: 470 mg/l (norm 440-540) → normal.
Additional diagnostic tests: Ferritin, transferrin saturation in case of anemia or fatigue symptoms.
ADMA / SDMA
Name: Asymmetric / symmetric dimethylarginine.
ADMA (asymmetric dimethylarginine) and SDMA (symmetric dimethylarginine) are degradation products of the amino acid arginine.
- ADMA inhibits the formation of nitric oxide (NO) → can constrict blood vessels and is a risk marker for cardiovascular diseases.
- SDMA influences arginine transport and is excreted via the kidneys → a marker for kidney function.
Significance: Marker of endothelial NO production (vasoregulatory).
Interpretation: ADMA 0.35 (< 0.66) → normal; SDMA 0.80 (> 0.35) → elevated, indicating impaired NO metabolism or renal strain.
Additional diagnostic tests: kidney function, arginine/citrulline status.
lactate
Name: Lactate in capillary blood.
Meaning: Marker for anaerobic energy production and mitochondrial function.
Interpretation: 6450 µmol/l (normal range 1490–5440) → elevated.
Indication of possible mitochondrial dysfunction or oxidative stress.
Additional diagnostics: BHI+ (Biovis Health Index), lactate/pyruvate ratio, coenzyme Q10.
Arginine / Citrulline
Name: Amino acids of the urea cycle.
Significance: NO production, ammonia detoxification, blood circulation.
Interpretation: Arginine 2.0 (< 4.45) → decreased; Citrulline 10.2 (normal) → indication of an unfavorable ratio, NO deficiency.
Additional diagnostic tests: L-arginine/citrulline ratio, SDMA, NO markers.
Glutamine / Glycine / Asparagine group
Name: Glucogenic amino acids.
Importance: Energy and glucose metabolism, immune system, gut health.
Interpretation: Glutamine 50 (< 92) → severely reduced; Glycine 302 → ok; Asparagine 50 → ok; → indication of energy deficiency or catabolism.
Additional diagnostics: mitochondrial parameters, amino acid profile trend.
Tryptophan / Kynurenine
Name: Serotonin/IDO axis.
Significance: Mood, stress balance, immune/inflammatory activity.
Interpretation: Tryptophan 31 (normal), Kynurenin 2.0 (> 1.2) → elevated, IDO activity ↑ (2.0 ratio > 49 normal) → indication of chronic inflammatory stimulus.
Additional diagnostic tests: hs-CRP, cortisol, vitamin B6 (status of tryptophan metabolism).
Omega-3 fatty acids (EPA/DHA)
Name: Eicosapentaenoic acid + Docosahexaenoic acid.
Significance: Inflammation modulation, cell membranes, heart/brain function.
Interpretation: EPA 1.62% (< 2) and DHA 3.2% (< 6) → significant deficiency.
Omega-3 index 0.51 (> 8**) → severely reduced.
Additional diagnostics: Re-examination after 3 months of Omega-3 supplementation; AA/EPA ratio (4.97 → good < 8).
Bile acid metabolism
Designation: Primary, secondary and tertiary bile acids.
Significance: Fat absorption, liver-intestinal signaling pathways, microbiome activity.
Interpretation: Total GS 1.2 µmol/l → normal; secondary/primary ratio 1.2 → physiological; no toxic dominance.
Additional diagnostics: Microbiome analysis (7α-dehydroxylase activity).
Glutamic acid
Meaning / Description:
Glutamic acid (glutamate) is the most important excitatory neurotransmitter and precursor of GABA; involved in energy and brain metabolism.
Interpretation:
Normal range (216–441) – balanced neurotransmitter and energy levels.
Additional diagnostics:
GABA, glutamine, cortisol, vitamin B6.
Carnitine
Meaning / Description:
Carnitine transports fatty acids into the mitochondria and is essential for energy production.
Interpretation:
At 22.3 µmol/l, it is within the normal range (18.2–47.5). A deficiency can lead to muscle weakness, fatigue, and reduced fat burning.
Additional diagnostics:
Acylcarnitine profile, coenzyme Q10, glucose, lactate, amino acid profile.
Phenylalanine
Meaning / Description:
Amino acid, precursor of tyrosine, dopamine, adrenaline and noradrenaline – important for mood, motivation and concentration.
Interpretation:
A level of 50 µmol/l is within the normal range (30–60). Values that are too high may indicate liver dysfunction or phenylketonuria, while values that are too low may indicate insufficient protein intake.
Additional diagnostics:
Tyrosine, tryptophan, liver parameters (ALT, AST), neurotransmitter profile.
Tyrosine
Meaning / Description:
Amino acid and precursor for dopamine, adrenaline, noradrenaline and thyroid hormones.
Interpretation:
Normal range (29–68) – borderline low, which may indicate increased consumption due to stress or insufficient protein intake.
Additional diagnostics:
Phenylalanine, TSH, cortisol, dopamine metabolites (HVA), nutritional analysis.
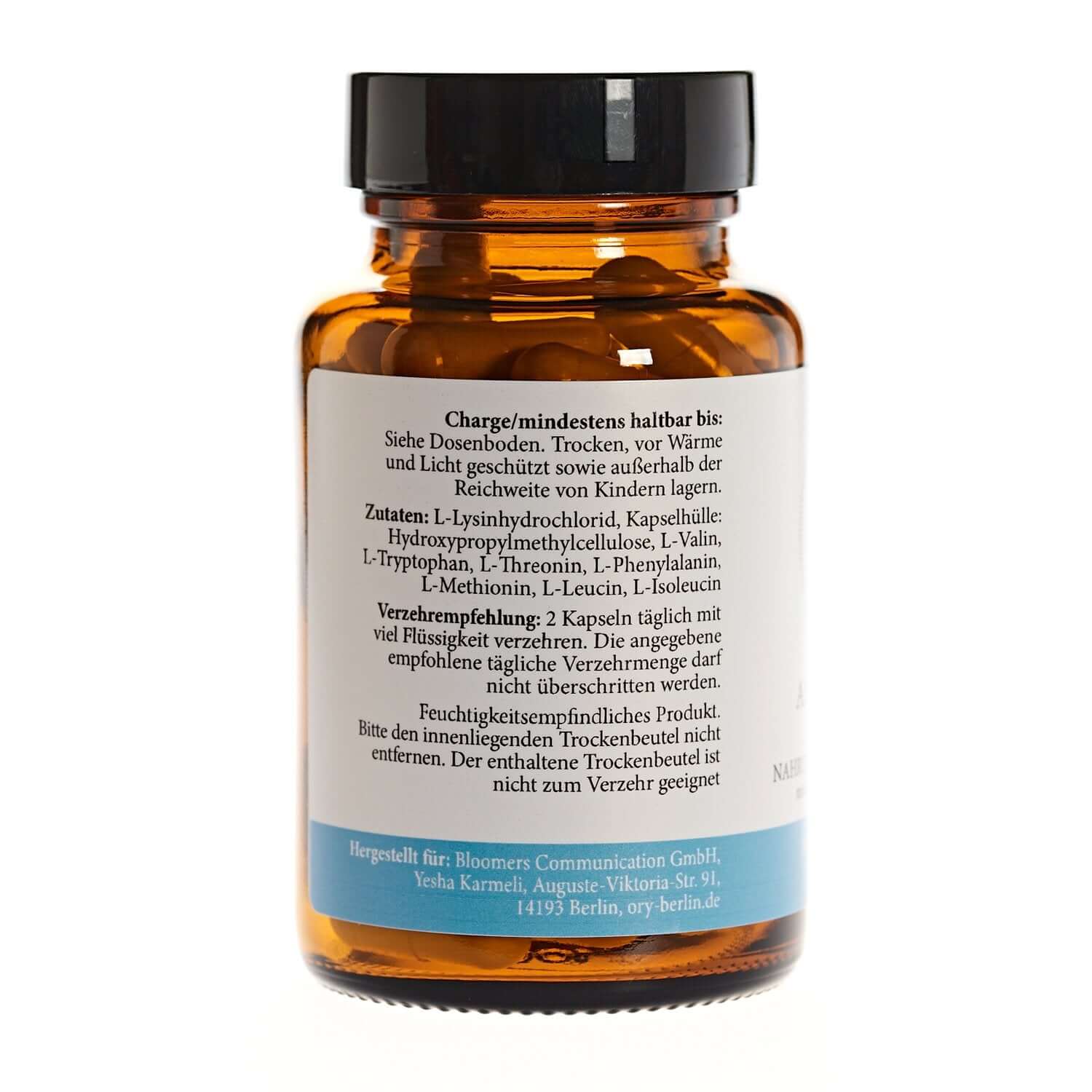
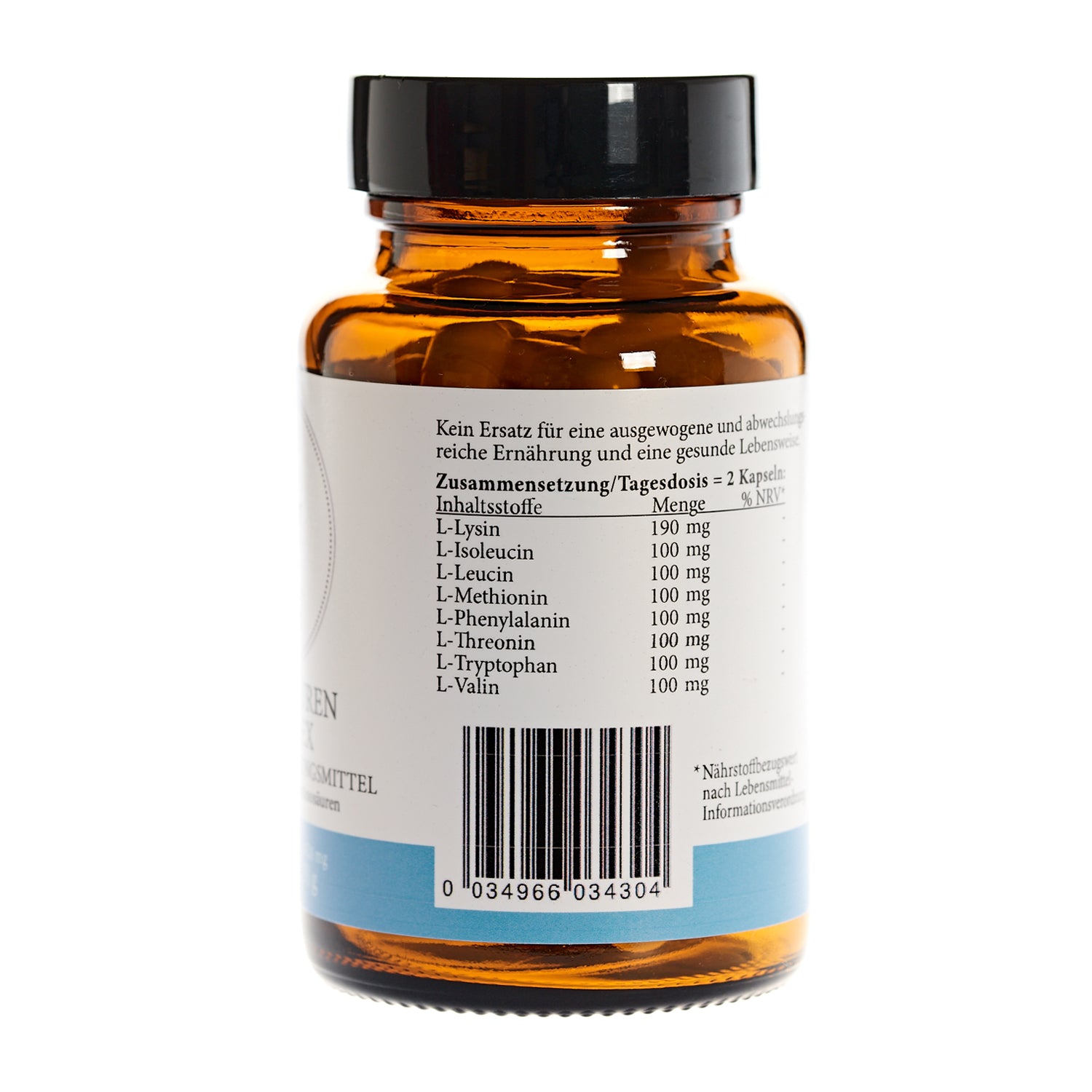
Valin
Meaning / Description:
Essential branched-chain amino acids (BCAAs), important for muscle building, energy and tissue regeneration.
Interpretation:
A level of 200.5 µmol/l is within the normal range (105–208). Stable amino acid status. Values that are too low indicate a catabolic metabolic state.
Additional diagnostics:
Leucine, isoleucine, total BCAAs, urea cycle parameters.
Choline
Meaning / Description:
Choline is an essential substance for the formation of cell membranes and neurotransmitters (e.g., acetylcholine). It supports liver function, memory, and fat metabolism.
Interpretation:
With a level of 66.0 µmol/l, the normal range (19.7–72) indicates good supply. A deficiency can lead to poor concentration, fatty liver, or muscle weakness.
Additional diagnostics:
Betaine (oxidation product of choline), homocysteine, liver enzymes (GPT, GOT).
Histidine
Meaning / Description:
Histidine is a semi-essential amino acid, a precursor of histamine, and important for immune function, wound healing, and pH regulation.
Interpretation:
With a level of 80 µmol/l, it falls within the normal range (42–89). Adequate supply argues against histamine intolerance.
Additional diagnostics:
Histamine, DAO (diamine oxidase), vitamin B6.
histamine
Meaning / Description:
Histamine is a biogenic amine that plays a role in inflammation, allergies, and gastric acid secretion.
Interpretation:
Reference range 0.4–0.92. This suggests histamine intolerance or increased mast cell activity. Symptoms may include skin redness, headaches, stomach upset, or sleep disturbances.
Additional diagnostics:
DAO activity, vitamin B6, methylhistamine in urine, mast cell activity (tryptase).
GABA (gamma-aminobutyric acid)
Meaning / Description:
GABA is the most important inhibitory neurotransmitter in the brain and has a relaxing, anxiety-reducing and sleep-promoting effect.
Interpretation:
Reference range 0.32–0.95. Indication of stress, lack of sleep or imbalance in neurotransmitter levels.
Additional diagnostics:
Glutamate/GABA ratio, cortisol, serotonin, vitamin B6 (cofactor of GABA synthesis).
Isoleucine
Meaning / Description:
Essential amino acid (BCAA), important for muscle growth, regeneration and blood sugar regulation.
Interpretation:
Normal range 32–7). Normal protein intake and muscle metabolism.
Additional diagnostics:
Leucine, valine, urea, creatinine.
Leucin
Meaning / Description:
Essential amino acid, stimulates muscle growth via activation of the mTOR signaling pathway.
Interpretation:
Normal range 56–117. Indication of a slight increased need, e.g. during physical exertion or diet.
Additional diagnostics:
Isoleucine, valine, total protein, urea cycle.
Betaine
Meaning / Description:
Betaine is produced from choline and is important for methylation processes, homocysteine degradation and cell protection.
Interpretation:
(Reference 17-52. Indication of impaired methyl metabolism or liver function. Consequences may include elevated homocysteine levels, fatty liver, and inflammation.)
Additional diagnostics:
Homocysteine, vitamin B12, folic acid, choline, liver enzymes (GOT, GPT).
Spermidine
Meaning / Description:
Spermidine is a polyamine that promotes cell regeneration, autophagy, and longevity. It supports cell growth, memory performance, and heart health.
Interpretation:
Normal range (1.7–6.7) – supply is sufficient, but can be improved. Low values occur during aging processes or oxidative stress.
Additional diagnostics:
Spermine, putrescine, oxidative stress markers, diet (spermidine-rich diet: wheat germ, soy, mushrooms).
Citrulline
Meaning / Description:
Citrulline is an amino acid of the urea cycle and serves to detoxify ammonia; it is also a precursor of arginine.
Interpretation:
Normal range (9.4–29.9) – stable, but at the lower end. Low values may indicate intestinal mucosal damage or low protein absorption.
Additional diagnostics:
Arginine, ornithine, plasma ammonia, liver parameters.
Arginine
Meaning / Description:
Arginine is a semi-essential amino acid, important for NO production, blood circulation, wound healing and immune function.
Interpretation:
Reference 4.45–27.2. Indication of reduced NO metabolism, impaired vascular function or high inflammatory activity.
Additional diagnostics:
Citrulline, ADMA, SDMA, nitrate/nitrite, blood pressure, homocysteine.
Threonine
Meaning / Description:
Essential amino acid, important for mucosal structure, immune defense and collagen formation.
Interpretation:
Normal range (51–123). Mild undersupply is possible in cases of increased need or protein deficiency.
Additional diagnostics:
Total protein, lysine, proline, digestive enzymes, gut microbiome.
Tryptophan
Meaning / Description:
Essential amino acid, precursor to serotonin and melatonin, important for mood, sleep and mental stability.
Interpretation:
Normal range (18.5–36). Normal status; decreased values would indicate stress, inflammation, or increased IDO activity.
Additional diagnostics:
Kynurenine, Serotonin, Vitamin B6, Cortisol, DHEAS.
Kynurenine
Meaning / Description:
Kynurenine is produced from tryptophan via the IDO enzyme cascade and is associated with inflammatory, immune and stress responses.
Interpretation:
Reference < 1.20. Indication of an activated immune response or chronic stress with increased IDO activity. This can lower serotonin levels and promote mood effects.
Additional diagnostics:
Tryptophan, kynurenine/tryptophan ratio (IDO activity), cortisol, CRP, interleukin-6.
IDO activity (kynurenine/tryptophan ratio)
Meaning / Description:
It provides information about the relationship between tryptophan breakdown and immune activity. A high value indicates inflammation or oxidative stress.
Interpretation:
(Reference 18–49) significantly reduced. This does not suggest inflammatory activation. IDO activity is inactive – serotonin production is likely unaffected.
Additional diagnostics:
Tryptophan, serotonin, cortisol, vitamin B6, inflammatory marker (CRP).
Cortisol
Meaning / Description:
Cortisol is the main stress hormone of the adrenal cortex, regulating blood sugar, inflammation, energy and the immune system.
Interpretation:
Normal range (0.06–0.24) – physiological secretion. Elevated values indicate stress or inflammation, decreased values indicate adrenal fatigue.
Additional diagnostics:
Daily profile (salivary cortisol), DHEA-S, ACTH, blood sugar, thyroid hormones.
DHEA-S (dehydroepiandrosterone sulfate)
Meaning / Description:
DHEA-S is a steroid hormone of the adrenal glands, an antagonist of cortisol, has an antioxidant effect and influences energy, libido and stress resilience.
Interpretation:
Normal range (0.3–2.8). A balanced ratio to cortisol indicates good stress adaptation.
Additional diagnostics:
Cortisol/DHEA ratio, testosterone, estradiol, vitamin C, micronutrient status (zinc, magnesium).
Hippuric acid
Meaning / Description:
End product of the microbial metabolism of polyphenols and flavorings; marker for liver detoxification and intestinal flora activity.
Interpretation:
Normal range (3–63) – normal detoxification performance and microbiome activity.
Additional diagnostics:
Benzoic acid, bile acids, liver parameters (GGT, ALT).
p-Cresol sulfate
Meaning / Description:
A bacterial breakdown product of tyrosine; potentially nephrotoxic and pro-inflammatory in high concentrations.
Interpretation:
Normal range (1.24–49.4) – unremarkable. Elevated values would indicate intestinal dysbiosis or liver/kidney strain.
Additional diagnostics:
Indoxyl sulfate, creatinine, urea, microbiome analysis.
Indole-3-acetic acid (IAA)
Meaning / Description:
Tryptophan metabolite of the microbiome; influences inflammatory processes and the intestinal barrier.
Interpretation:
(Reference < 1.55) – Indication of intestinal dysbiosis or increased bacterial tryptophan utilization.
Additional diagnostics:
Tryptophan, indole propionic acid, microbiome analysis (e.g., gut flora sequencing).
Indolepropionic acid
Meaning / Description:
Microbial product with antioxidant and neuroprotective effects.
Interpretation:
Normal range (0.08–1.28) – healthy microbiome activity.
Additional diagnostics:
Indole-3-acetic acid, indoxyl sulfate, oxidative stress status.
Indoxyl sulfate
Meaning / Description:
A microbial tryptophan degradation product that can accumulate in renal insufficiency; a marker for the gut-kidney axis.
Interpretation:
Normal range (0.68–4.3) – unremarkable.
Additional diagnostics:
Creatinine, urea, p-cresol sulfate, microbiome status.
Putrescin
Meaning / Description:
A polyamine produced during protein breakdown by intestinal bacteria. Toxic in high quantities and an indicator of dysbiosis.
Interpretation:
(Reference < 0.22). Indicates increased microbial protein breakdown and intestinal imbalance.
Additional diagnostics:
Spermidine, spermine, gut microbiome profile, liver function.
Alanine
Meaning / Description:
Alanine is a glucogenic amino acid that can be converted to glucose in the liver and plays an important role in energy and blood sugar metabolism.
Interpretation:
Normal range (179–411) – adequate energy supply. Low values indicate energy deficiency or protein insufficient supply, high values indicate a catabolic metabolic state.
Additional diagnostics:
Asparagine, glutamine, blood sugar, insulin, lactate.
Asparagin
Meaning / Description:
Asparagine is involved in protein synthesis and energy production in the citric acid cycle; it is also important for the nervous system.
Interpretation:
Normal range (31.3–63.5) – unremarkable energy metabolism. Reduced values can occur in cases of protein deficiency or increased energy consumption (e.g., stress).
Additional diagnostics:
Aspartic acid, glutamine, urea, cortisol.
Aspartic acid
Meaning / Description:
Amino acid of the citric acid cycle, important for energy production, hormone formation and neurotransmission.
Interpretation:
Normal range (30.3–175) – no abnormalities. Low values indicate protein deficiency, high values indicate cell breakdown or acidosis.
Additional diagnostics:
Glutamate, ammonia, lactate, pH value.
Glutamine
Meaning / Description:
Glutamine is the most abundant amino acid in the blood, important for the gut, immune system, energy production and wound healing.
Interpretation:
(Reference 92–209). Indication of increased consumption due to stress, inflammation, catabolism, or tumor metabolism.
Additional diagnostics:
Ammonia, lactate, C-reactive protein (CRP), gut microbiome, total protein.
Glycine
Meaning / Description:
Glycine acts as an inhibitory neurotransmitter and is central to detoxification (glutathione), collagen formation and sleep quality.
Interpretation:
Normal range (186–416) – adequate supply. Low values may indicate detoxification disorder, oxidative stress, or liver strain.
Additional diagnostics:
Glutathione, homocysteine, methionine, liver enzymes (ALT, AST).
Lysine
Meaning / Description:
Essential amino acid for collagen and elastin formation, tissue repair and immune function.
Interpretation:
Normal range (36–85) – balanced protein status.
Additional diagnostics:
Threonine, proline, vitamin C (collagen synthesis), zinc.
Proline
Meaning / Description:
An amino acid required for collagen, skin, tendon and connective tissue formation.
Interpretation:
Normal range (89–228) – no abnormalities.
Additional diagnostics:
Lysine, vitamin C, hydroxyproline in urine (connective tissue breakdown).
Taurine
Meaning / Description:
Taurine is a sulfur-containing amino acid, important for the nervous system, heart, gallbladder, electrolyte balance and antioxidant cell protection.
Interpretation:
(Reference 96–196). Indication of oxidative stress, liver strain, bile acid or mitochondrial dysfunction.
Additional diagnostics:
Liver values (GGT, ALT, AST), glutathione, zinc, magnesium, vitamin B6.
Hormone profile (saliva test)
The saliva test measures the biologically active, free hormones (e.g., cortisol, DHEA, testosterone, progesterone, estradiol) – that is, those that are actually effective in the body.
It is used to assess the hormonal balance, especially in cases of exhaustion, stress, mood swings, sleep disorders, libido changes or hormonal imbalances.
Cortisol
Name: Cortisol (saliva)
Meaning/Description: Stress hormone of the adrenal cortex; among other things, it controls glucose metabolism, blood pressure, and inflammation inhibition (circadian rhythm).
Interpretation: (Norm 3–9) → within the normal range. Notes: Too high → acute stress, depression, Cushing's syndrome; too low → adrenal insufficiency, chronic fatigue (context needed).
Additional diagnostics: Daily profile (multiple saliva samples), serum cortisol ± ACTH, DHEA-S, possibly dexamethasone suppression test.
progesterone
Name: Progesterone (saliva)
Meaning/Description: Precursor of corticosteroids/androgens; present in low amounts in men, acts, among other things, as a neurosteroid.
Interpretation: (Norm 23.8–58) → at the upper end of the normal range. Clinically usually unremarkable; significantly elevated, e.g., with exogenous administration.
Additional diagnostics: In case of complaints: serum progesterone, medical history regarding supplements/creams, overall context with estradiol/testosterone.
Estradiol (E2)
Name: Estradiol (saliva)
Meaning/Description: Most potent estrogen; in men, it is primarily produced by the aromatization of testosterone; it affects libido, bones, and blood vessels.
Interpretation: Result 3.13 pg/ml (normal range 1.5–3.3) → in the upper normal range. Elevated levels are possible with increased aromatase activity, obesity, liver disease, or exogenous intake.
Additional diagnostic tests: Serum E2 (sensitive assay), SHBG, total testosterone + calculated free T, liver function tests; if necessary, aromatase risk factors (medication, alcohol, abdominal fat).
Progesterone/estradiol ratio (P/E ratio)
Name: P/E ratio (saliva) – calculated
Meaning/Description: Ratio of progesterone to estradiol as a rough indicator of balance.
Interpretation: (Reference 30–50) → significantly reduced (= relatively greater estrogenic effect compared to progesterone). Significance depends heavily on the clinical context (e.g., sleep, mood, weight, libido). 4. Additional diagnostics: Repeat check, serum levels (progesterone, E2), thyroid (TSH, fT3/fT4), liver function, body fat/metabolism (HbA1c, fasting insulin).
DHEA
Name: DHEA (saliva)
Meaning/Description: Adrenal androgen precursor; marker for adrenal reserve/stress resilience.
Interpretation: Result 202.28 pg/ml (normal range 140–570) → within the normal range (lower middle range). Low: chronic stress/age; high: supplementation, adrenal hyperfunction.
Additional diagnostics: Serum DHEA-S (stable marker), cortisol day profile, history of DHEA preparations.
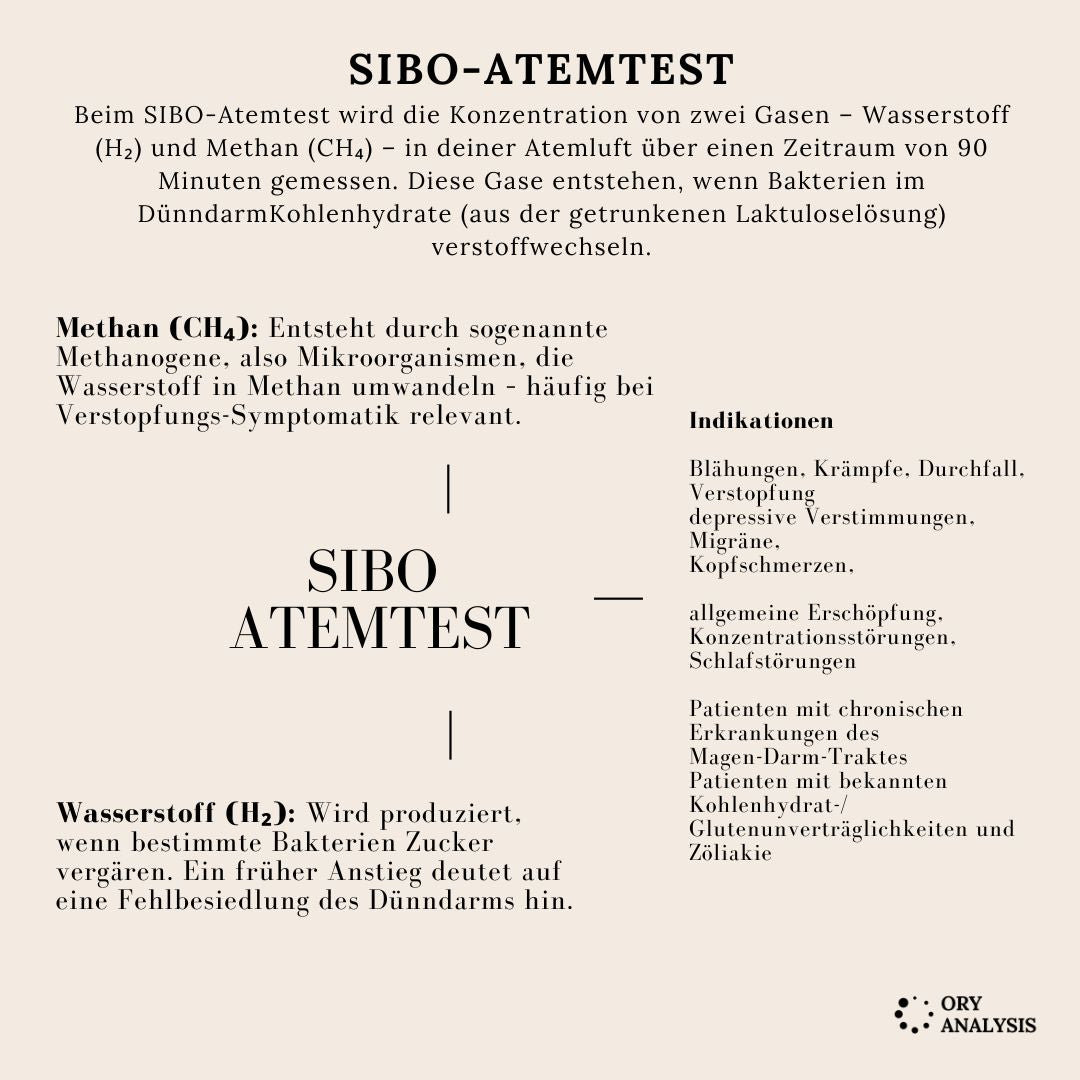
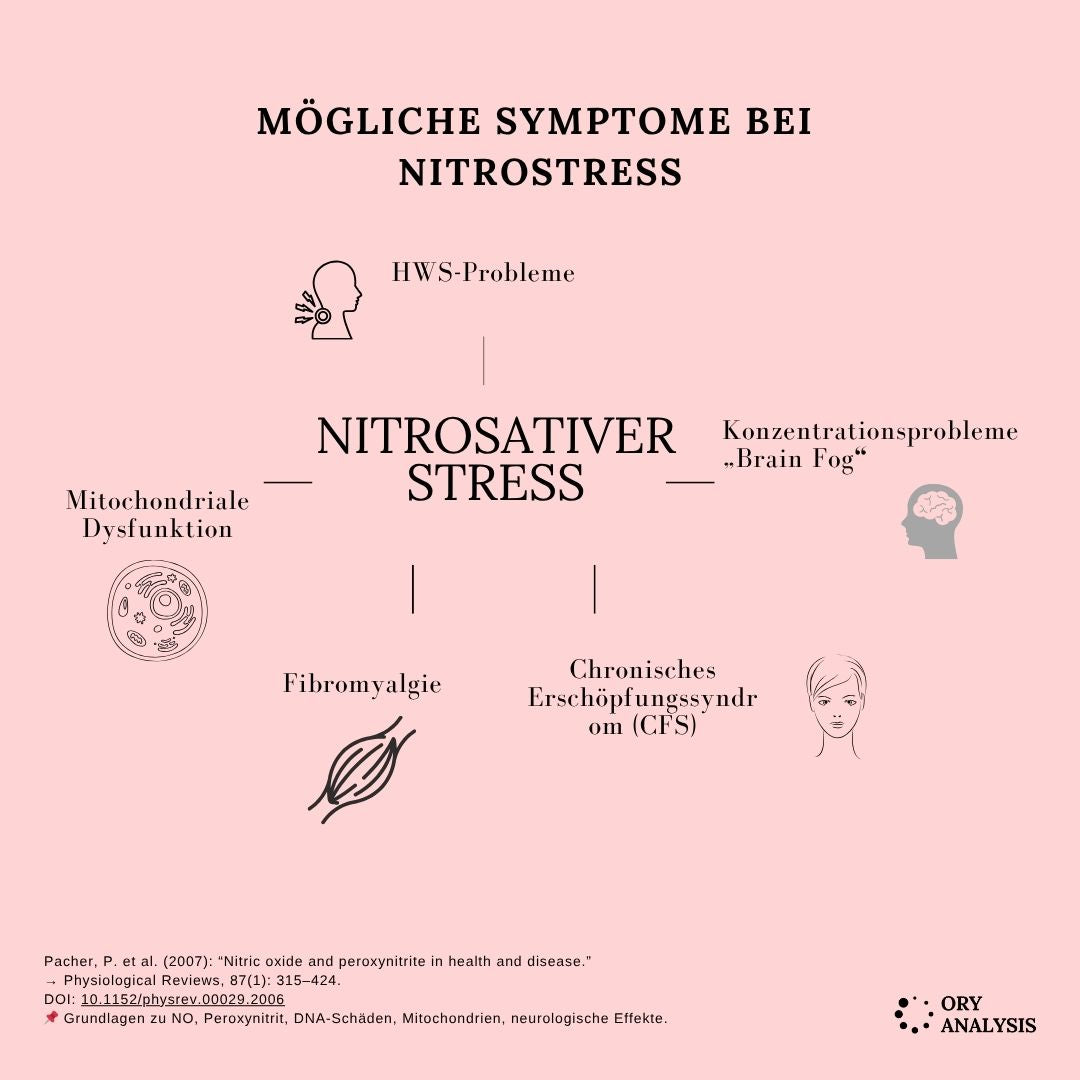
Nitrosative stress – cell stress profile (urine):
This test assesses oxidative and nitrosative cellular stress in the body. It reveals whether free radicals or nitrogen compounds are burdening cells, DNA, or mitochondria.
Early detection of cellular stress, B12 metabolism disorders and intestinal or mitochondrial function problems.
Advantages:
- Non-invasive (urine sample)
- Combines several important markers
- Provides information on oxidative damage, NO load, and energy/detoxification status
8-OH-Deoxyguanosine (8-OHdG)
Meaning / Description:
Marker for oxidative DNA damage; occurs when free radicals oxidize DNA bases. Elevated levels indicate increased oxidative stress.
Result: (Reference: < 9.68) → normal. Interpretation (too high / too low):
Too high: Oxidative stress ↑ (e.g., chronic inflammation, smoking, environmental toxins, intense exertion).
Too low: Clinically unremarkable; very low values are usually irrelevant. Additional diagnostics:
Total antioxidant status, GSH/GSSG ratio, coenzyme Q10, vitamin C/E, hs-CRP; lifestyle/exposure history.
4-Hydroxynitrophenylacetic acid
Meaning / Description:
Urinary metabolite used as an indicator of nitrosative stress (NO/peroxynitrite-related processes).
Result: (Reference: < 4.5) → low/normal.
Interpretation (too high / too low):
- Too high: Indications of nitrosative stress (e.g., chronic inflammation, infections, mitochondrial dysfunction).
- Low/normal: No indication of increased NO/ONOO⁻ exposure.
Additional diagnostics:
Nitrotyrosine, NO metabolites (nitrite/nitrate), homocysteine, BH4/BH2 balance (indirect), inflammatory markers (hs-CRP), mitochondrial function tests.
Methylmalonic acid (MMA)
Meaning / Description:
Functional marker for vitamin B12 status (adenosylcobalamin-dependent methylmalonyl-CoA mutase). Elevated in B12 deficiency or, less commonly, genetic enzyme defects/renal insufficiency.
Result: 1.78 mg/g creatinine (reference: < 2.3) → normal.
Interpretation (too high / too low):
- Too high: Suspected B12 deficiency, renal ↓ clearance, bacterial overgrowth (rare).
- Normal/low: No functional B12 deficiency is apparent.
Additional diagnostics:
Holotranscobalamin (Holo-TC), serum B12, homocysteine, folate, kidney function (creatinine/eGFR).
Citrulline
Meaning / Description:
Amino acid of the urea cycle; serves as a marker for enterocyte mass/small intestine function (e.g. reduced in case of mucosal damage).
Result: (Reference: < 4) → normal. (Note: The laboratory uses "< 4" as the cutoff value; in this context, the increase is primarily being evaluated.)
Interpretation (too high / too low):
- Reduced (in methods with lower reference values): possible small bowel mucosal atrophy, malabsorption.
- Elevated: rarely clinically relevant; may vary in urea cycle disorders.
- Citrulline in urine reflects the activity of the urea cycle and shows how efficiently ammonia is detoxified.
- Elevated levels may indicate a disruption of the urea cycle, impaired liver function, or increased protein breakdown.
- Low levels often indicate reduced liver function, a deficiency of ornithine or arginine, or mitochondrial dysfunction.
- In functional medicine, citrulline also serves as a marker for intestinal health, as it is produced in the enterocytes (small intestine cells) – low levels can indicate damage to the intestinal mucosa.
- Overall, citrulline testing helps to holistically assess liver, intestinal and mitochondrial function.
Additional diagnostics:
Amino acid profile (arginine, ornithine), ammonia, urea, intestinal diagnostics (in case of symptoms), inflammatory markers.
Creatinine (urine, enzymatic)
Meaning / Description:
Its primary purpose here is to normalize creatinine levels in relation to other urine markers (compensating for fluctuations in concentration/fluctuations in fluid intake).
Result: (Reference: 290–2260) → within the reference range.
Interpretation (too high / too low):
- Low: Diluted urine (high fluid intake).
- High: Concentrated urine (low fluid intake).
Additional diagnostics:
In case of abnormalities: serum creatinine/eGFR, urinalysis.
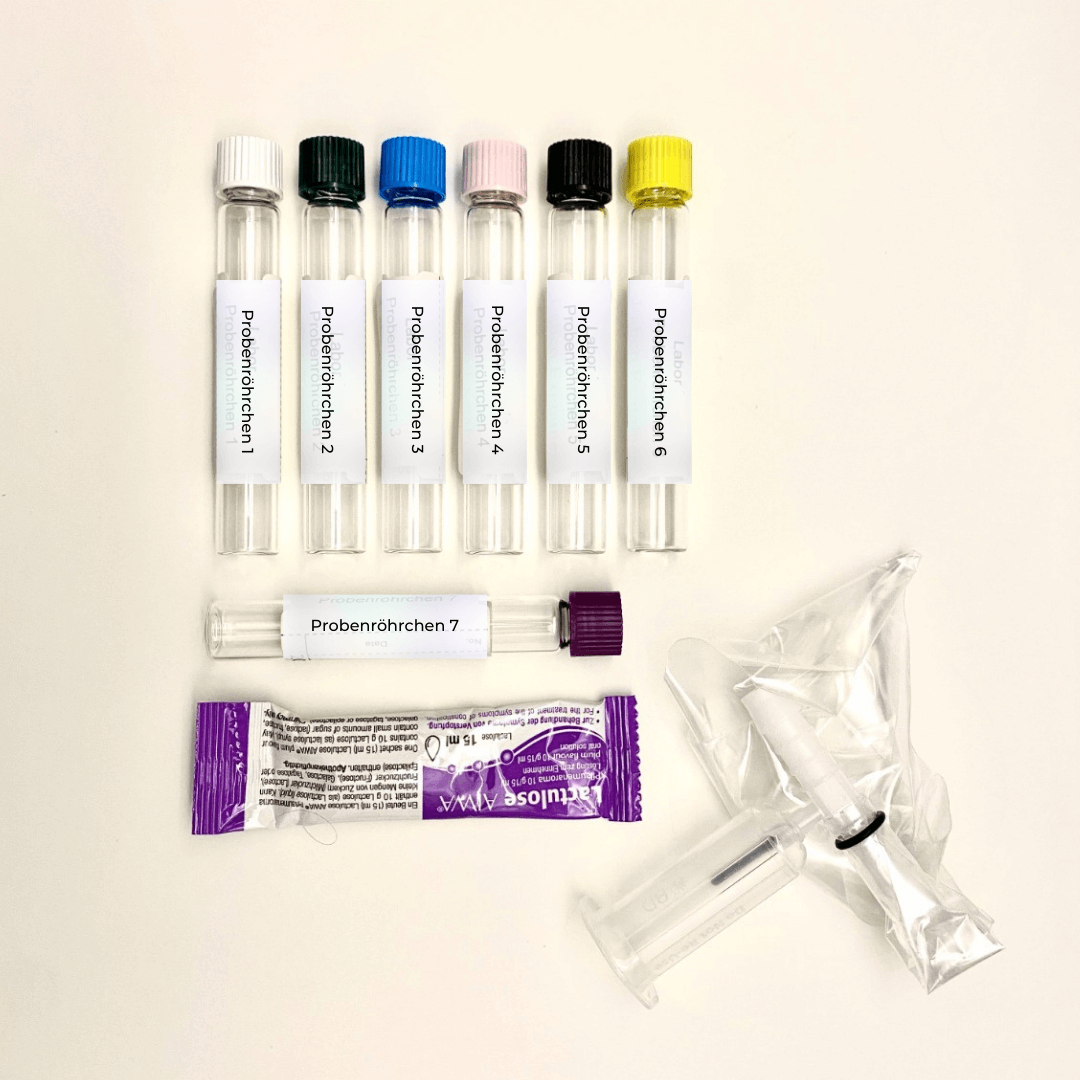
The BASIS-GUT test (with Akkermansia profile)
It examines the composition and function of the intestinal flora, digestive performance and intestinal mucosal barrier.
Purpose of the test:
It is used to assess intestinal health, digestion, and immune defense. This allows for the early detection of dysbiosis, bacterial imbalances, digestive weaknesses, mucosal disorders, or inflammatory processes.
Advantages:
- Holistic overview of microbiota, digestive residues, inflammation and barrier function
- Detects overgrowth or deficiency of beneficial bacteria (e.g., bifidobacteria, akkermansia)
- Provides information on nutrient absorption, leaky gut risk, and immune status
- Supports therapy planning for digestive problems, food intolerances, skin or metabolic issues.
In short:
👉 The test shows how well the gut functions, whether the flora is balanced and whether the intestinal mucosa remains healthy – an important basis for digestion, immune system and general well-being.
Aerobic bacteria
Name: Escherichia coli
Significance: Leading germ, marker for gut ecology.
Interpretation: 1.0 × 10⁷ CFU/g — upper limit of normal (Ref. 10⁶–10⁷). 4) Additional diagnostics: In case of symptoms: Dysbiosis profile over time, check diet/prebiotics.
Name: Klebsiella spp.
Meaning: Potential pathobiont/opportunist.
Interpretation: 1.0 × 10⁷ CFU/g — significantly elevated (ref. <10⁴). Indication of dysbiosis/overgrowth. 4) Additional diagnostics: Follow-up monitoring, antibiotic history, if clinically relevant, further pathogen diagnostics/antibiogram.
Name: Enterococcus spp.
Meaning: Commensal lactic acid bacteria.
Interpretation: <1.0×10⁴ CFU/g — significantly reduced (Ref. 10⁶–10⁷). 4) Additional diagnostics: Consider diet (fiber), pro-/synbiotic strategy; monitor course.
Names: Proteus, Pseudomonas, Enterobacter, Serratia, Hafnia spp.
Meaning: Opportunists.
Interpretation: all low/<detection limit — within the target range.
Additional diagnostics: monitoring of disease progression, antibiotic history, possibly extended germ diagnostics/antibiogram if clinically relevant.
Anaerobic bacteria
Name: Bifidobacterium spp.
Importance: Key microbiota (fermenters, SCFA).
Interpretation: (Ref. 10⁹–10¹¹).
Additional diagnostics: Prebiotic dietary fiber (inulin/fructans depending on tolerance), monitoring of progress.
Name: Bacteroides spp.
Meaning: Dominant anaerobes, protein/fat breakdown.
Interpretation: Normal range (10⁹–10¹¹), rather in the lower third of the normal range.
Additional diagnostics: Check fiber quality; monitor progress.
Name: Lactobacillus spp.
Importance: Lactic acid producer, pH stabilization.
Interpretation: (Ref. 10⁵–10⁷).
Additional diagnostics: Testing fermented foods/targeted probiotics; monitoring progress.
Name: Clostridium spp. (total)
Meaning: Heterogeneous group.
Interpretation: <1.0×10⁵ CFU/g — within the target range (Ref. <10⁵). 4) Additional diagnostics: None, if asymptomatic.
Mycology
- Candida spp. – collective term for various Candida species
- Candida albicans – the most common pathogenic Candida species
- mold – e.g. B. Aspergillus, Penicillium, Mucor
- Geotrichum – a type of yeast, sometimes pathogenic in immunocompromised individuals.
Meaning
- These are opportunistic pathogens, meaning they usually only cause infections when the immune system is weakened or the barrier function is impaired.
- Candida albicans: typically causes mucosal infections (mouth, genitals, intestines)
- Geotrichum: rare, but possible in cases of immunodeficiency
- Mold fungi: inhalant → lungs, systemic → dangerous in immunocompromised individuals
interpretation
- Negative/below threshold = unremarkable, no indication of current pathogenic mycoses
- Normal colonization is possible, especially with yeasts in the gut4) Additional diagnostics (in case of suspected relevant fungal load or immunodeficiency)
If clinical relevance is suspected (e.g., recurrent infections, chronic complaints, unclear symptoms), the following should be considered.
Diagnostic steps that are useful:
A) Check immune status
- Differentiated blood count analysis
- Leukocytes, lymphocyte subgroups (CD4/CD8), neutrophils, monocytes
- Immunoglobulins (IgA, IgG, IgM, IgE)
- Cytokine status (e.g. IL-6, TNF-α)
Indication of inflammatory activity or dysregulation
- T-cell function tests (in cases of unclear immunodeficiency)
B) Gut microbiome & mucosal barrier (in case of Candida finding in stool) - Microbiome analysis (stool)
- Composition, diversity, yeast load, short-chain fatty acids
- Zonulin (stool/serum)
- Marker for intestinal permeability (“Leaky Gut”)
- sIgA (secretory IgA in stool)
- Immune defense in the mucous membrane
C) Specific fungal diagnostics (in case of clinical suspicion) - Fungal PCR or culture (depending on location – stool, vaginal swab, sputum, etc.)
- (1,3)-β-D-glucan in serum
- Markers for systemic fungal infections (especially in the case of mold)
- Aspergillus antigen (galactomannan)
When is additional diagnostic testing particularly useful in cases of suspected invasive aspergillosis?
- Recurrent infections (especially Candida)
- Chronic fatigue, "brain fog", skin problems, digestive issues
- History of antibiotic use → disrupted microbiome
- Autoimmune diseases
- Immunosuppressive therapies (cortisone, chemotherapy)
- Diabetes mellitus
Stool pH value
Designation
pH value in stool → measures whether the intestinal contents are more acidic or alkaline.
Meaning
- The pH reflects the microbiological fermentation behavior:
- Acidic pH (5.5–6.5) → sign of healthy carbohydrate fermentation by lactic acid bacteria and bifidobacteria (e.g., formation of short-chain fatty acids such as butyrate, acetate).
- Alkaline pH (>7.0) → indicates increased protein degradation processes (proteolysis) and a shift towards putrefactive flora.
interpretation
- Your value: 7.3 → slightly alkaline, above the reference range (5.8–6.5).
- Possible causes:
- Low fiber intake → fewer plant fibers for the "good" gut bacteria.
- High protein content (e.g., meat, shakes) → promotes putrefactive bacteria (Clostridia, Bacteroides).
- Reduced carbohydrate fermentation → less lactic acid production → pH increases.
- Antibiotic therapy or dysbiotic flora following stress/illness.
Consistency and color of the chair
Designation
Visual assessment of consistency (firm, soft, mushy, liquid) and color (brown, light brown, dark, grey, green, black, yellow).
Meaning
These characteristics provide clues about:
- Digestive performance (fat utilization, bile acid flow)
- Transport time in the intestine
- Diet
- Possible pathologies (malabsorption, cholestasis, bleeding, etc.)
interpretation
- Mushy, light brown → mostly nonspecific, often functional or nutritional in nature.
- Light brown: normal to slightly faster intestinal transit, less bile influence.
- Loose stool: may indicate a higher water content in the stool (e.g., due to a high-fiber or high-fat diet, mild maldigestion, or stress).
A single finding without symptoms → not pathological.
In case of chronic loose stools, check for causes such as food intolerances (lactose, fructose, FODMAPs), bile acid loss, pancreatic insufficiency or irritable bowel syndrome.
Digestive residue examination
Quantitative fat in stool
Label: Quantitative fat in stool
Significance: Provides information about fat digestion and absorption in the intestine. → Especially important for detecting disorders of fat absorption (e.g., due to intestinal diseases) or pancreatic insufficiency (pancreatic insufficiency).
Interpretation:
(Reference: < 3.5 g/100 g) → This means: There is slightly more fat in the stool than normal, i.e., minimal fat maldigestion or malabsorption. → This is called subtle steatorrhea (mild fatty stools, often without visible fat deposits).
Possible causes:
- Slightly reduced pancreatic elastase (pancreas produces too few digestive enzymes)
- Too high a diet or certain types of fat (e.g., MCT- or Omega-3-rich foods) • rapid intestinal transit (e.g., in cases of irritable bowel syndrome, infections)
- Bile acid deficiency or loss (in cases of gallbladder problems)
Additional diagnostics: → Food diary (check fat quantity/type) → Monitoring during the course of treatment → If symptoms persist: pancreatic elastase in stool or 72-hour fat balance for more precise quantification.
Quantitative sugar in stool
Label: Quantitative sugar in stool
Meaning: Does not measure "table sugar", but rather unabsorbed carbohydrates (especially disaccharides or monosaccharides). → Indication of carbohydrate malabsorption (e.g., lactose, fructose, or sorbitol intolerance).
Interpretation: (Ref.: < 2.5 g/100 g) → More sugar residues remain in the stool than usual. → These are fermented by bacteria in the large intestine, which can lead to gas, bloating, diarrhea, or abdominal pain.
Possible causes:
- Lactose intolerance (milk sugar is not completely broken down)
- Fructose malabsorption
- too high a proportion of fermentable carbohydrates (FODMAPs)
- Rapid intestinal transit or small intestinal bacterial overgrowth (SIBO)
Additional diagnostic tests: → H₂ breath tests (for lactose, fructose, sorbitol) → possibly FODMAP dietary analysis → possibly stool flora analysis for chronic conditions
Quantitative nitrogen and water
Name: Quantitative nitrogen, water
Meaning:
- Nitrogen: Measure of protein breakdown products in stool → shows whether protein is poorly digested or not absorbed (e.g. in cases of inflammation, maldigestion).
- Water: Provides information about the water content of the stool → relevant in cases of diarrhea or constipation.
Interpretation:
- Nitrogen: 0.50 g/100 g – normal (< 1.0)
- Water: 80 g/100 g – normal (75–85)→
This means: Protein digestion is normal, no signs of malabsorption or inflammation. → The stool water content is also physiological, i.e., neither diarrhea nor excessively dry stool.
Additional diagnostic testing: → None required, as the results were unremarkable.
Overall rating:
Slightly elevated fat and sugar residues indicate mild digestive weakness — possibly due to:
short-term dietary factors (e.g., high-fat, low-fiber, or high-FODMAP meals),
- functional disorders (irritable bowel syndrome with rapid passage),
- or incipient enzyme deficiencies (e.g., pancreas, lactase).
If you have symptoms such as bloating, fatty stools, diarrhea or a feeling of fullness, targeted further diagnostic testing would be advisable.
Maldigestion - Pancreatic elastase/Bile acids
Pancreatic elastase
Meaning:
Pancreatic elastase is an enzyme produced exclusively by the exocrine pancreas and excreted in the stool. It serves as a marker for exocrine pancreatic function, i.e., the pancreas's ability to provide digestive enzymes.
Interpretation:
(>200 µg/g)
→ The value is within the normal range and indicates normal exocrine pancreatic function.
- >200 µg/g: normal function
- 100–200 µg/g: mild to moderate insufficiency
- <100 µg/g: severe exocrine pancreatic insufficiency
Comment:
A normal value practically rules out relevant pancreatic insufficiency as a cause of maldigestion.
Additional diagnostics:
The examination should only be repeated or supplemented (e.g., by imaging procedures such as sonography or MRCP) if there is clinical suspicion or for monitoring purposes (e.g., newly occurring fatty stools, weight loss, chronic diarrhea).
Bile acids (stool)
Meaning:
The determination of bile acids in stool is used to assess bile acid malabsorption syndrome or impaired bile acid reabsorption in the terminal ileum.
Bile acids are important for fat digestion; impaired reabsorption can lead to chronic diarrhea and fatty stools.
Interpretation:
(<70 µmol/l)
→ The value is within the normal range and argues against bile acid loss or malabsorption.
Comment:
A normal stool bile acid level largely rules out bile acid malabsorption, especially if there is no clinically evident chronic diarrhea or fat malabsorption.
Additional diagnostics:
In cases of persistent chronic diarrhea and continued clinical suspicion, a functional study may be considered as an additional measure.
Diagnostic procedures are performed:
- SeHCAT test (nuclear medicine, measures bile acid reabsorption)
- Serum C4 determination (marker for bile acid synthesis in the liver) Overall assessment:
Both parameters (pancreatic elastase and bile acids in stool) are within the normal range.
→ No evidence of maldigestion or malabsorption due to pancreatic insufficiency or bile acid loss.
However, if clinical symptoms such as bloating, diarrhea, or weight loss persist, further investigations should be carried out to rule out other causes, e.g.: - Small intestinal bacterial overgrowth (SIBO breath test)
- Celiac disease (serology: transglutaminase Ab, IgA)
- Lactose / fructose intolerance
- Microscopic colitis
Malabsorption / Inflammation
Tests for calprotectin and alpha-1-antitrypsin in stool are used to assess inflammation and barrier function of the intestinal mucosa.
- Calprotectin indicates whether there is inflammatory activity in the intestine (e.g., in Crohn's disease, ulcerative colitis, infections).
- Alpha-1 antitrypsin checks whether protein is lost through the intestinal mucosa or whether the intestinal barrier is damaged.
Calprotectin (stool)
Significance: Calprotectin is a protein found predominantly in neutrophils. It serves as a sensitive marker for inflammatory processes in the intestinal mucosa. Elevated levels indicate activation of the immune system in the gastrointestinal tract, as can occur in chronic inflammatory bowel diseases (e.g., Crohn's disease, ulcerative colitis) or infectious enteritis.
Result / Interpretation: normal (< 50 mg/l). The measured value is within the normal range. Therefore, there is no indication of relevant inflammatory activity of the intestinal mucosa at the time of the examination.
Additional diagnostics / recommendation: In the case of persistent gastrointestinal symptoms (e.g. diarrhea, abdominal pain, weight loss), follow-up monitoring may be useful in order to detect changes in the inflammatory process at an early stage.
In case of clinical suspicion of inflammatory bowel disease, further diagnostic testing may be necessary (e.g. colonoscopy, CRP determination).
Alpha-1 antitrypsin (stool)
Significance: Alpha-1-antitrypsin is a protein found in serum that is hardly excreted into stool when the intestinal mucosa is intact. It serves as a marker for impaired intestinal barrier function or for protein loss via the intestine (enteral protein-losing syndromes).
Result / Interpretation: (< 27.5 mg/dl). The value is within the normal range. There is no indication of increased intestinal permeability or relevant enteral protein loss.
Additional diagnostics / recommendation:
In case of persistent symptoms or suspected malabsorption syndrome, follow-up monitoring or additional diagnostic tests (e.g. stool elastase, pancreatic function tests, H2 breath tests) may be considered.
Mucosal immunity & barrier
Name: sIgA (secretory immunoglobulin A)
Meaning:
Secretory IgA is the most important antibody of the mucosal immune defense. It is produced by plasma cells in the lamina propria and secreted into the intestinal lumen via epithelial cells.
sIgA binds to antigens, microorganisms, and toxins, thereby preventing their adhesion to the mucosa ("immune exclusion"). It thus serves as a key marker of mucosal immunocompetence.
Interpretation:
Value: (Reference: 510–2040 µg/ml).
→ Indication of an intact secretory immune defense of the intestinal mucosa.
Additional diagnostics:
Follow-up monitoring is only necessary in the presence of clinical symptoms (e.g., recurrent infections, chronic inflammatory bowel diseases, food intolerances). If values remain persistently low or significantly elevated, further immunological or microbiological testing should be performed.
Zonulin (chair)
Meaning:
Zonulin is a physiological regulator of tight junctions in the intestinal epithelium. It controls the permeability of the epithelial barrier.
Elevated zonulin levels are interpreted as an indication of increased intestinal permeability (“leaky gut syndrome”) and can occur in various inflammatory, autoimmune or metabolic diseases.
Interpretation:
Value: (Reference: < 55 ng/ml).
→ There is no evidence of impaired barrier function of the intestinal mucosa.
Additional diagnostics:
In cases of persistent clinical symptoms (e.g., bloating, diarrhea, food intolerances, chronic inflammation), a supplementary assessment of other barrier or inflammatory markers (e.g., alpha-1-antitrypsin, calprotectin, serum lipopolysaccharide-binding protein) may be useful.
Histamine (stool)
Histamine is a biogenic amine that acts as a messenger substance in the body – including in the immune system, the nervous system and the gastrointestinal tract.
It is produced both by the body itself (e.g. in mast cells) and by certain bacteria in the intestine.
Meaning:
An elevated histamine level in the stool may indicate histamine exposure or microbial dysbiosis (imbalance of the intestinal flora).
- Some intestinal bacteria (e.g. Morganella, Proteus, Klebsiella, Enterobacter) produce histamine.
- Stress, intestinal inflammation, increased permeability of the intestinal wall (leaky gut) or an unbalanced diet can increase local histamine production.
- Furthermore, a deficiency of histamine-degrading enzymes (e.g., diamine oxidase – DAO) can worsen the situation.
Interpretation:
Normal value: < 200 ng/ml → low/normal
- A value below this limit does not indicate a relevant histamine load.
- Values above 200 ng/ml may indicate increased activity of histamine-producing intestinal bacteria or a reduced degradation capacity.
In some laboratories, an increase up to about 950 ng/ml is described as mild to moderate exposure, while values above this are considered significantly elevated.
However, the exact assessment depends on the laboratory results and the clinical symptoms.
Additional diagnostics:
An isolated measurement in the stool is usually not sufficient for diagnosis.
Useful additional examinations (only in the case of corresponding symptoms such as headache, skin redness, digestive problems, fatigue, etc.) include:
- DAO activity in the blood (serum): → Reduced values indicate a limited ability to break down histamine from food.
- Histamine in plasma or urine: → Provides indications of systemic (whole-body) histamine levels.
- Gut flora analysis (microbiome): → Can show whether histamine-producing bacteria are overrepresented.
- Dietary history: → Histamine-rich foods (e.g., red wine, cheese, sausage, canned fish, tomatoes, spinach) and food reactions (IGG test) often lead to symptoms.
- Stress diagnostics : → Chronic stress can activate mast cells and increase histamine release.
Mucin/butyrate formation
Faecalibacterium prausnitzii
Name: Faecalibacterium prausnitzii
Meaning:
- One of the most important butyrate producers in the human intestine.
- Butyrate (butyric acid) is a short-chain fatty acid that serves as the main energy source for intestinal epithelial cells (colonocytes).
- It has an anti-inflammatory effect by inhibiting NF-κB signaling pathways and promoting regulatory T cells.
- A high proportion is associated with an intact intestinal mucosa, lower susceptibility to inflammation and better metabolic balance.
Interpretation:
- Reference range: > 5.0 × 10¹⁰ CFU/g
- Rating: Very good – above the reference value. → Indication of stable butyrate production and a favorable microbial environment.
Additional diagnostics / recommendations:
- Maintain dietary fiber diversity: Different plant fibers promote microbial diversity.
- Particularly beneficial: resistant starch (e.g., cooled potatoes/rice), inulin, pectins, oat β-glucans.
- Continue to monitor chronic inflammation (e.g., IBD, irritable bowel syndrome with a tendency to inflammation) over time.
- A decline is possible with antibiotic therapy – consider preventive nutrition or probiotic support if necessary.
Akkermansia muciniphila
Name: Akkermansia muciniphila
Meaning:
- A key representative of mucin layer-associated bacteria.
- It breaks down mucin (a component of the intestinal mucosa) in a controlled manner and simultaneously stimulates mucus production – important for mucosal integrity and barrier function.
- It has beneficial effects on metabolism, body weight, blood sugar regulation and inflammation balance.
- Reduced concentrations are associated with obesity, type 2 diabetes, fatty liver disease and chronic inflammatory bowel diseases.
Interpretation:
- Reference range: > 1.5 × 10¹⁰ CFU/g
- Assessment: Slightly reduced – indication of possible impairment of the mucosal barrier or reduced mucin layer activity.
Additional diagnostics / recommendations:
Polyphenol-rich foods: e.g., berries, green tea, pomegranate, grapes, red cabbage.
Prebiotics: Inulin, fructooligosaccharides (FOS), resistant starch promote Akkermansia.
Periods of fasting or moderate calorie reduction can promote population growth.
Avoid excessive sugar, saturated fats and alcohol, as these can inhibit Akkermansia.
Follow-up examinations are recommended after approximately 3–6 months, especially in case of clinical symptoms (e.g. mucosal irritation, bloating, signs of dysbiosis).
Summary of the microbiological situation:
- Butyrate production: very well developed → anti-inflammatory, protective environment.
- Mucin layer stability: slightly impaired → starting point for nutritional and lifestyle-related optimization.
Cortisol daily profile in saliva
Cortisol is the body's most important stress hormone, produced in the adrenal cortex. It reflects the daily rhythm of adrenal gland activity – normally high in the morning and low in the evening. Saliva measurement shows the biologically active (free) cortisol fraction.
Cortisol daily profile in saliva
Meaning / Description
Cortisol is the body's most important glucocorticoid (stress hormone) and is produced in the adrenal cortex (zona fasciculata).
It is regulated via the hypothalamic-pituitary-adrenal (HPA) axis:
- The hypothalamus releases CRH (corticotropin-releasing hormone).
- This stimulates the pituitary gland to release ACTH (adrenocorticotropic hormone).
- ACTH then stimulates the adrenal cortex to produce cortisol.
Cortisol exhibits a distinct daily rhythm (“circadian rhythm”):
- The level is highest in the morning (shortly after waking up) to activate the body.
- It slowly drops around midday.
- The value is lowest in the evening/at night, so that the body can rest.
Saliva measurement is particularly informative because it only measures the free, biologically active cortisol – that is, the amount that actually acts in the tissue (as opposed to total cortisol in serum, which is also bound to transport proteins).
Cortisol levels – high or low:
An elevated cortisol level means that the body is under stress or strain – either acute (short-term) or chronic (long-term).
Cortisol is released in stressful situations to provide energy and make the body “ready to fight”.
Possible causes:
- Psychological or physical stress
- Lack of sleep or irregular sleep
- Overload, chronic stress, anxiety
- Inflammation, infections, pain
- Overactive adrenal glands (e.g., Cushing's syndrome)
- Certain medications (e.g., cortisone preparations)
Effects of a persistently high cortisol level:
- Elevated blood sugar and cravings (especially for sweets)
- Weight gain (especially around the abdomen)
- Elevated blood pressure
- Sleep disturbances and restlessness
- Concentration problems, irritability, mood swings
- Weakened immune system (susceptibility to infection)
- Muscle loss, thinner skin, slowed wound healing
- Menstrual irregularities in women, loss of libido
In the short term, an elevated cortisol level is normal and even vital, e.g. in the morning when waking up or during acute exertion.
However, persistently high levels are unhealthy and lead to exhaustion and regulatory disorders.
When cortisol is too low:
A low cortisol level means that the body is producing too little of the stress hormone or that the adrenal glands are exhausted or underactive.
This can occur after prolonged periods of stress, when the adrenal glands are "burned out" and can no longer provide enough cortisol.
Possible causes:
- Chronic stress over a long period → “Adrenal fatigue”
- Adrenal insufficiency (Addison's disease) • Pituitary gland disorder (too little ACTH)
- Prolonged cortisone therapy (suppression of endogenous production)
- Hypoglycemia or very restrictive diets
- Lack of sleep or persistent exhaustion
Effects of low cortisol levels: - Severe fatigue and lack of motivation
- Low blood pressure, dizziness upon standing
- Low blood sugar, trembling, weakness
- Difficulty concentrating
- Depressive mood, irritability
- Low stress tolerance ("small things quickly cause stress")
- Increased tendency towards inflammation, weak immune system
A cortisol level that is too low means that the body can no longer react adequately to stress – stress resistance is reduced, and those affected often feel exhausted or “empty”.
Additional diagnostic testing (for clarifying the cause: cortisol day profile)
Additional diagnostic testing (to clarify the causes)
- DHEA in saliva or serum → ratio to cortisol shows balance between “stress and regeneration hormones”.
- Serum ACTH → indicates whether the control by the pituitary gland is functioning correctly.
- Cortisol awakening response (CAR test) → measures the increase within the first 30–45 minutes after waking, very sensitive for stress regulation.
- Stress hormone profile (adrenaline, noradrenaline, dopamine in 24-hour urine) → shows sympathetic activation.
- Thyroid parameters (TSH, fT3, fT4) → important, as cortisol and thyroid hormones influence each other.
Effects of cortisol in the body
Cortisol is a vital hormone with a very broad effect throughout the entire organism.
It is often referred to as the "stress hormone" because it is released in increased amounts during stressful situations to enable the body to adapt and react quickly. However, its effects extend far beyond stress.
In metabolism, cortisol ensures that the body has sufficient energy available. It increases the production of new glucose in the liver (gluconeogenesis), inhibits the effect of insulin, and thus promotes higher blood sugar levels. This is beneficial in stressful situations because the brain and muscles then receive more energy. However, if cortisol levels remain elevated over a prolonged period, this can lead to:
- Weight gain, especially in the abdominal area,
- and lead to insulin resistance.
- Cortisol has a suppressive effect on the immune system.
- It suppresses inflammation and excessive immune responses. Therefore, it is often used medically as an anti-inflammatory or immunosuppressant drug (e.g., cortisone).
- However, persistently high cortisol levels can weaken the immune system, which increases susceptibility to infection or slows wound healing.
- In the cardiovascular system, cortisol supports blood pressure regulation.
- It ensures that the blood vessels can respond appropriately to other hormones such as adrenaline.
- However, excessively high cortisol levels over a prolonged period can lead to high blood pressure .
- In the brain, cortisol increases alertness, attention, and concentration.
- In the short term, it helps to think clearly and react quickly.
- However, if the level is chronically elevated, this can lead to nervousness, irritability , sleep disorders or depressive moods.
- In muscles and bones, cortisol has a catabolic effect: it promotes the breakdown of muscle protein to produce sugar and inhibits bone formation.
- Therefore, in the long term, excessively high cortisol levels can promote muscle loss or osteoporosis .
Cortisol also has a significant influence on mental health. - In acute stress phases, it promotes motivation, focus and performance.
- However, prolonged stress and exhaustion can cause cortisol production to decrease – then you feel tired, lethargic and emotionally exhausted.
What do persistently abnormal cortisol levels mean?
Cortisol levels can fluctuate significantly depending on life circumstances, stress levels, and health status. What's important is not so much a single measurement, but rather the pattern throughout the day and over a longer period.
If cortisol levels are consistently too high or too low, this can indicate various disorders of stress regulation.
Persistently elevated cortisol levels often indicate a sustained activation of the stress system. This means the body is constantly "on high alert" —even when there is no actual immediate danger. Causes can include chronic psychological or physical stress, overwork, lack of sleep, emotional strain, or inflammatory processes in the body. In such cases, the HPA axis remains overactive, and cortisol is continuously released.
In the long term, this can lead to symptoms such as inner restlessness, sleep disorders, concentration problems, weight gain (especially in the abdominal area), increased blood pressure, irritability and a weakened immune system.
Depressive moods or a so-called "burnout" state can also be associated with chronically elevated cortisol levels. In rare cases, pathologically elevated levels can also be caused by hormonal disorders, such as Cushing's syndrome (overactive adrenal cortex or an ACTH-producing tumor).
Persistently low cortisol levels, on the other hand, can indicate adrenal fatigue or a weakening of the pituitary gland's control mechanism. This often occurs after prolonged periods of stress, when the body is "burned out" and can no longer properly adjust cortisol production.
People with low cortisol levels often feel very tired, lethargic, and exhausted. They frequently suffer from low blood pressure, dizziness, difficulty concentrating, and increased sensitivity to stress. Hypoglycemia, muscle weakness, and depressive moods can also occur. Severe adrenal insufficiency is called Addison's disease – however, this is rare and requires medical treatment.
Generally speaking, a balanced cortisol rhythm – high in the morning, low in the evening – is crucial for energy, performance, good sleep, and emotional stability. Deviations from this rhythm indicate that the stress response system is out of balance. Depending on the direction (too high or too low), this can be a sign of overexertion or exhaustion and should be investigated further by a doctor, especially if symptoms persist.