ORY Praevent
ORY Praevent – Prevention begins with diagnostics

Diagnostics as prevention – together with you for greater regenerative capacity
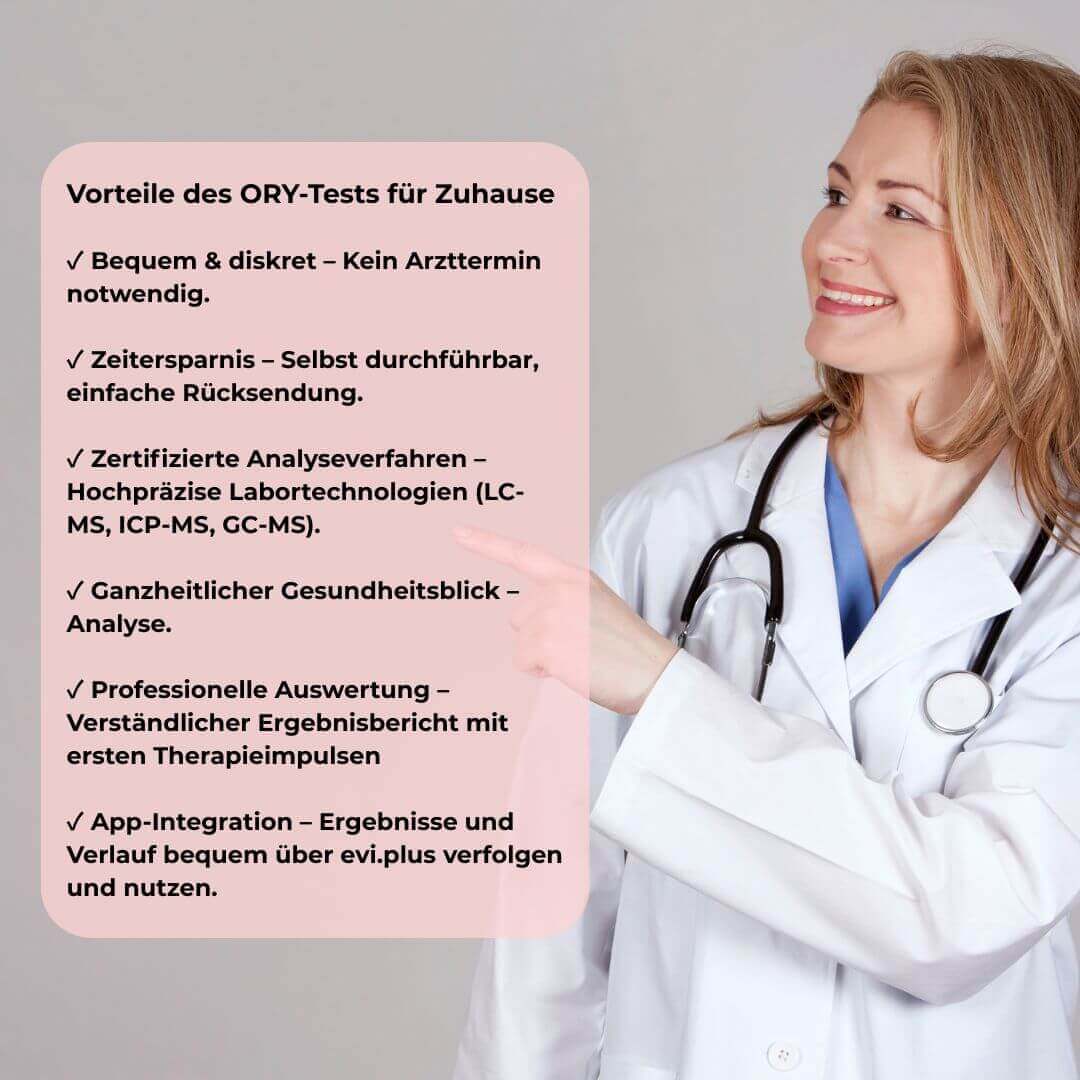
Integrate preventive diagnostics into your practice. ORY Praevent strengthens regeneration and therapy success through data-based analysis and app feedback.
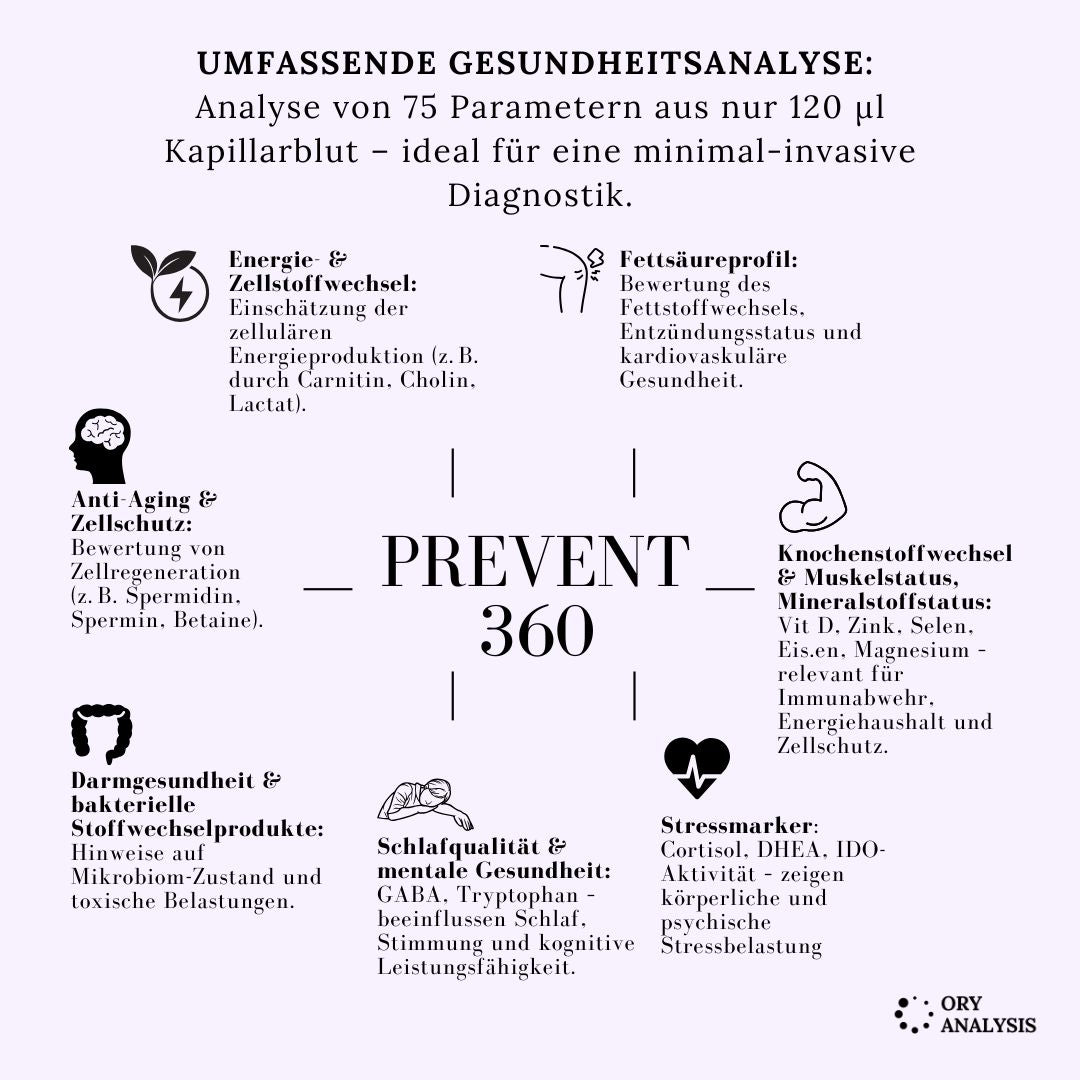
Diagnostics for regenerative medicine and prevention.
Many medical procedures, therapies, or chronic illnesses place demands on the body beyond its current performance and regulatory capacity. A lack of physical, metabolic, or physiological capacity increases the risk of complications and prolongs recovery time.
Targeted diagnostic screening in advance allows for the identification of critical weaknesses, targeted intervention, and improved regenerative capacity. Your practice can thus assume a valuable preventative function – supporting medical treatment and increasing patient safety.
Your added value as a partner
Based on the data, we support your patients with evidence-based recommendations (nutrition, exercise, micronutrients, stress management), tailored to their individual situation.
You will receive well-founded diagnostic data from your patients (e.g., via blood, laboratory, vital parameters, metabolic, inflammatory or regeneration markers).
You strengthen your medical quality and differentiation by integrating an additional prevention service.
How it works
1.
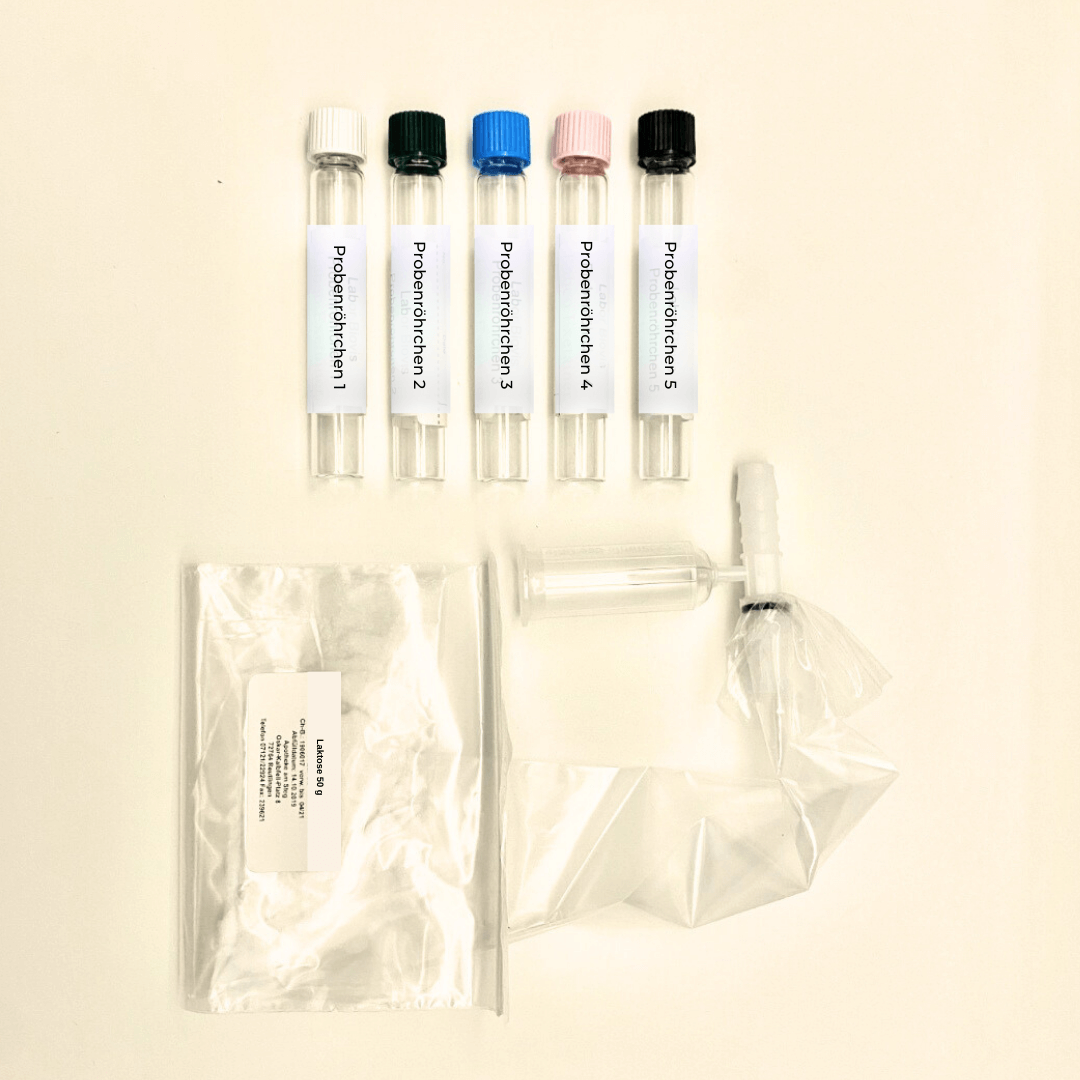
Invitation & Diagnostics
They recommend diagnostic screening to their patients (e.g., before surgery, in cases of chronic diseases, as an additional service).
2.
Analysis & Feedback
The samples/measurements are evaluated → the data is made accessible via app (for the patient and you).
3.
Support & Optimization
We provide concrete recommendations for action; your practice can adapt individually based on the data, and further diagnostics can take place during the course of treatment.

Who would benefit from this?
- Dentists, before major procedures (implants, jaw reconstructions, etc.)
- Surgeons (Orthopedics, Visceral Surgery, Cardiovascular)
- Doctors with chronically ill patients (e.g., metabolic disorders, autoimmune diseases, chronic inflammation)
- Therapists who provide long-term care for patients (e.g., physiotherapy, naturopathic treatments, complementary medicine)
Evidence-based research proves that nutrient deficiencies slow down healing processes and hinder the body's regeneration.
Nutritional deficiencies slow down healing processes and tissue regeneration. Micronutrients are essential for cell growth, energy production, and immune response. Studies show that targeted supplementation and dietary adjustments promote recovery. Preventive diagnostics enable timely detection and intervention. - brief, scientifically sound, with a concise study summary
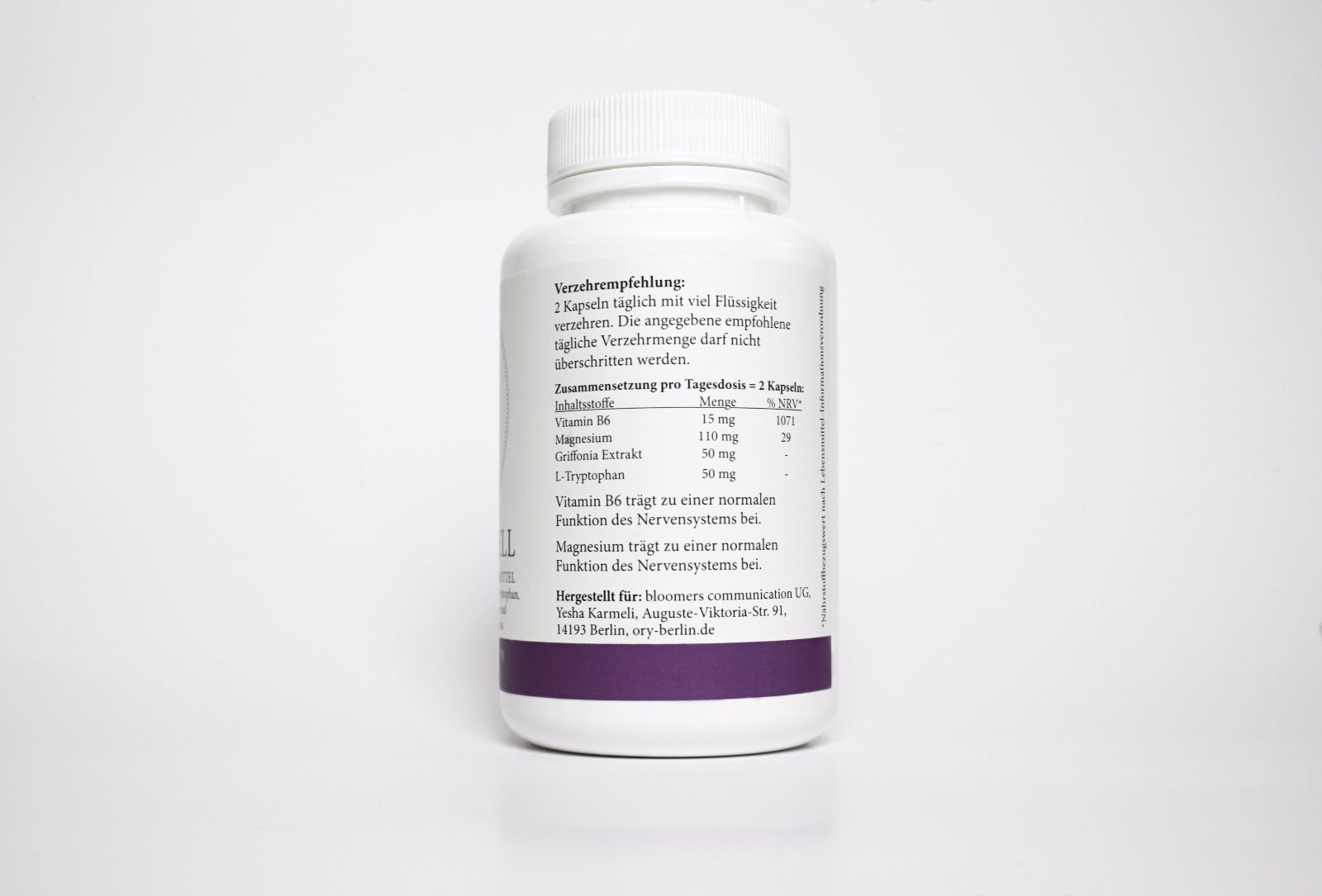
A deficiency in B vitamins
Vitamin B1, B6, and B12 (especially) impair neuronal regeneration, as these vitamins are necessary for myelination, energy metabolism, and antioxidant defense. A deficiency can lead to permanent nerve degeneration, pain, and peripheral neuropathy.
Vitamin D deficiency
Vitamin D deficiency is associated with muscle weakness, reduced muscle regeneration, and an increased risk of falls; supplementation improves muscle regeneration after injuries and surgeries.
Vitamin E deficiency
Vitamin E deficiency leads to impaired nerve regeneration and a reduction in the types of muscle cells needed for repair.
Vitamin A deficiency
Vitamin A deficiency alters the composition of the extracellular matrix and impairs cell proliferation and differentiation, disrupting tissue repair.
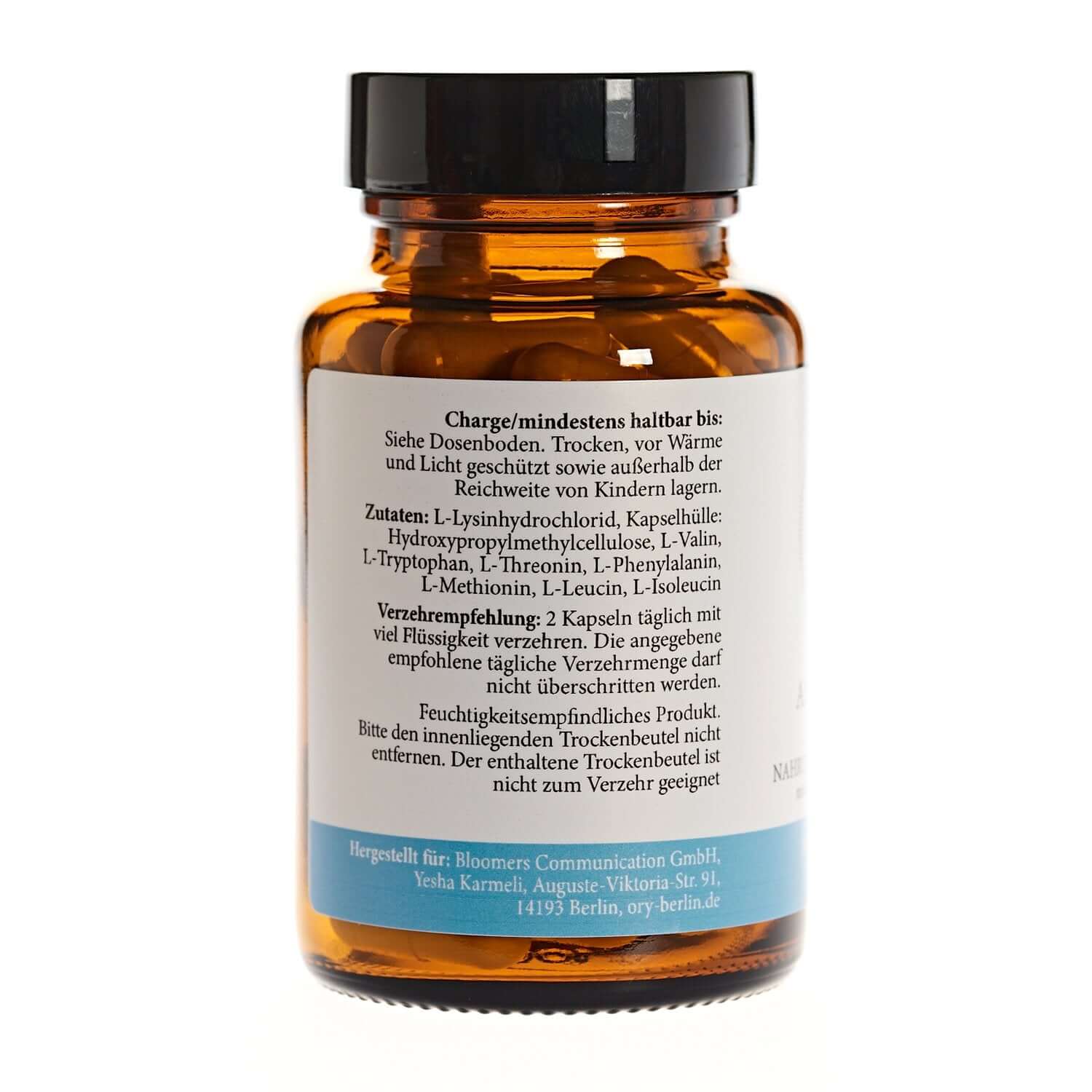
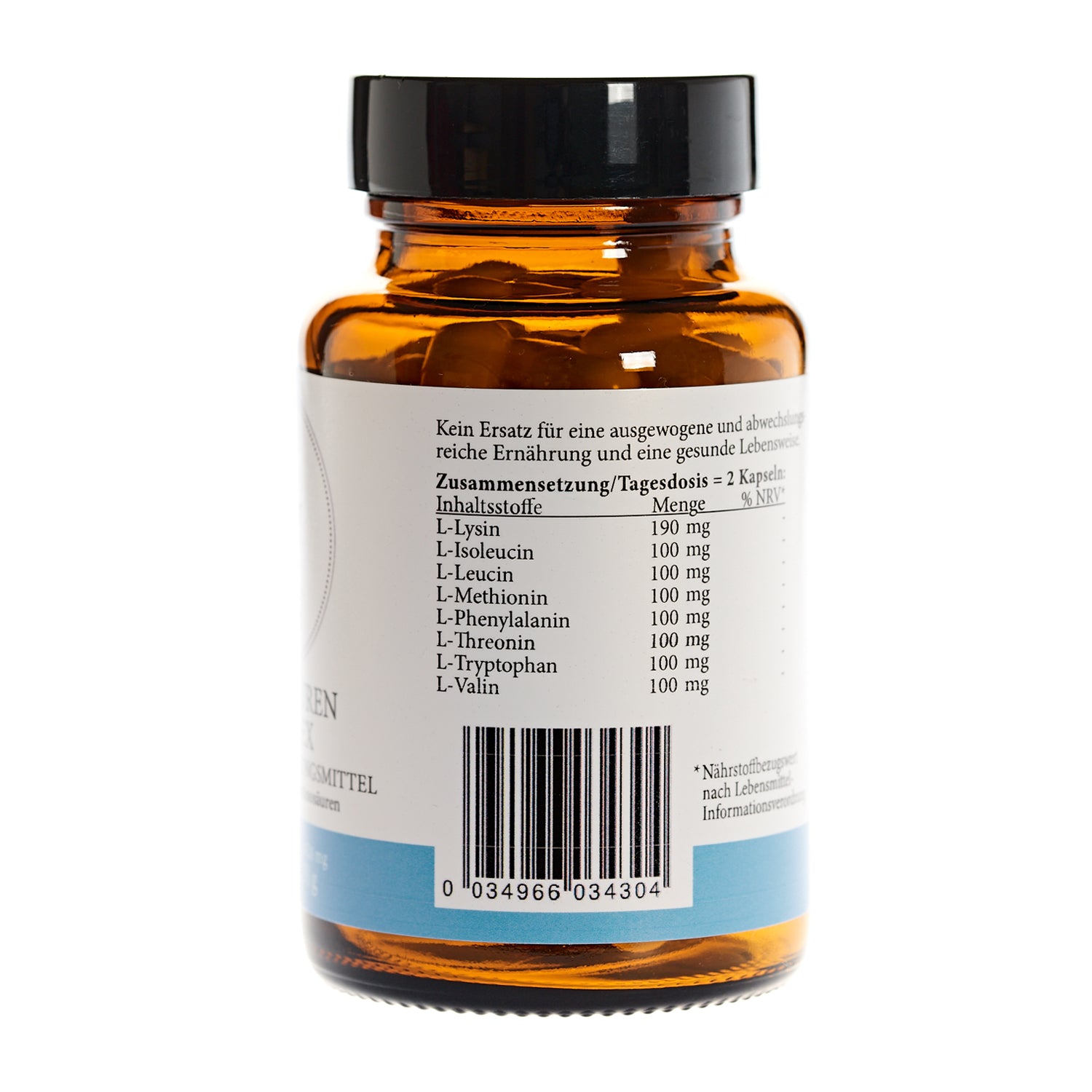
amino acid deficiency
Amino acid deficiency – especially of essential and conditionally essential amino acids such as arginine and glutamine – limits protein synthesis, inhibits cell proliferation, and impairs immune function. This leads to delayed or incomplete regeneration of muscle, nerve, and organ tissue.
Cardiovascular complications:
Elevated homocysteine levels in cases of vitamin B12 or folic acid deficiency are associated with an increased risk of thromboembolic events.
Thiamine deficiency can lead to Wernicke encephalopathy and beriberi, vitamin E deficiency to spinocerebellar ataxia, vitamin A deficiency to visual impairment, and vitamin D deficiency to osteomalacia.
Neurological disorders:
Vitamin B12 deficiency can lead to sensory ataxia, peripheral neuropathy, myelopathy (subacute combined degeneration of the spinal cord), cognitive impairment, and psychiatric symptoms. These neurological manifestations can precede hematological symptoms and are potentially irreversible if not treated promptly.
Hematological complications: Vitamin B12 and folic acid deficiency cause megaloblastic anemia with increased susceptibility to infection, fatigue, dyspnea and, in severe cases, pancytopenia.
Central nervous system disorders, immunodeficiency and impaired wound healing:
Central nervous system disorders: Deficiencies in certain amino acids (e.g., serine, proline, glutamine) can lead to microcephaly, developmental delay, seizures, spasticity, and polyneuropathy. In adults, spastic paraplegia and polyneuropathies are the most prominent.
Arginine and glutamine deficiency impairs immune function and delays wound healing, especially in critically ill patients.
Muscle weakness and protein breakdown: Chronic amino acid deficiency leads to muscle atrophy, hypoalbuminemia and an increased risk of infection.
ORY OneCare Prevent – Prevention begins with diagnostics
Become a partner now & offer diagnostics for your patients
*Evidence-based research
Stabler SP. The New England Journal of Medicine. 2013;368(2):149-60. doi:10.1056/NEJMcp1113996.
Green R, Miller JW. Vitamins and hormones. 2022;119:405-439. doi:10.1016/bs.vh.2022.02.003.
3. Cobalamin Deficiency: Clinical Picture and Radiological Findings.
Briani C, Dalla Torre C, Citton V, et al.
Nutrients. 2013;5(11):4521-39. doi:10.3390/nu5114521.
4. Alterations in Sulfur Amino Acids as Biomarkers of Disease.
Stabler SP. The Journal of Nutrition. 2020;150(Suppl 1):2532S-2537S. doi:10.1093/jn/nxaa118.
5. Cobalamin, Folic Acid, and Homocysteine.
Varela-Moreiras G, Murphy MM, Scott JM.
Nutrition Reviews. 2009;67 Suppl 1:S69-72. doi:10.1111/j.1753-4887.2009.00163.x.
Leading Journal
6. ACG Clinical Guideline: Malnutrition and Nutritional Recommendations in Liver Disease.
Singal AK, Wong RJ, Dasarathy S, et al.
The American Journal of Gastroenterology. 2025;120(5):950-972. doi:10.14309/ajg.0000000000003379.
Practice Guideline New Research
Gwathmey KG, Grogan J. Muscle & Nerve. 2020;62(1):13-29. doi:10.1002/mus.26783.
8. Vitamin Deficiencies in Children: Lessons From Clinical and Neuroimaging Findings.
Dupuy G, Roux CJ, Barrois R, et al.
European Journal of Pediatric Neurology : EJPN : Official Journal of the European Pediatric Neurology Society. 2024;50:6-15. doi:10.1016/j.ejpn.2024.02.013.
9. Amino Acid Synthesis Deficiencies.
de Koning TJ. Journal of Inherited Metabolic Disease. 2017;40(4):609-620. doi:10.1007/s10545-017-0063-1.
10. Acquired Amino Acid Deficiencies: A Focus on Arginine and Glutamine.
Morris CR, Hamilton-Reeves J, Martindale RG, Sarav M, Ochoa Gautier JB.
Nutrition in Clinical Practice: Official Publication of the American Society for Parenteral and Enteral Nutrition. 2017;32(1_suppl):30S-47S. doi:10.1177/0884533617691250.
11. Amino Acid Homeostasis and Signaling in Mammalian Cells and Organisms.
Bröer S, Bröer A. The Biochemical Journal. 2017;474(12):1935-1963. doi:10.1042/BCJ20160822.