INTESTINAL MICROBIOME CHECK-UP
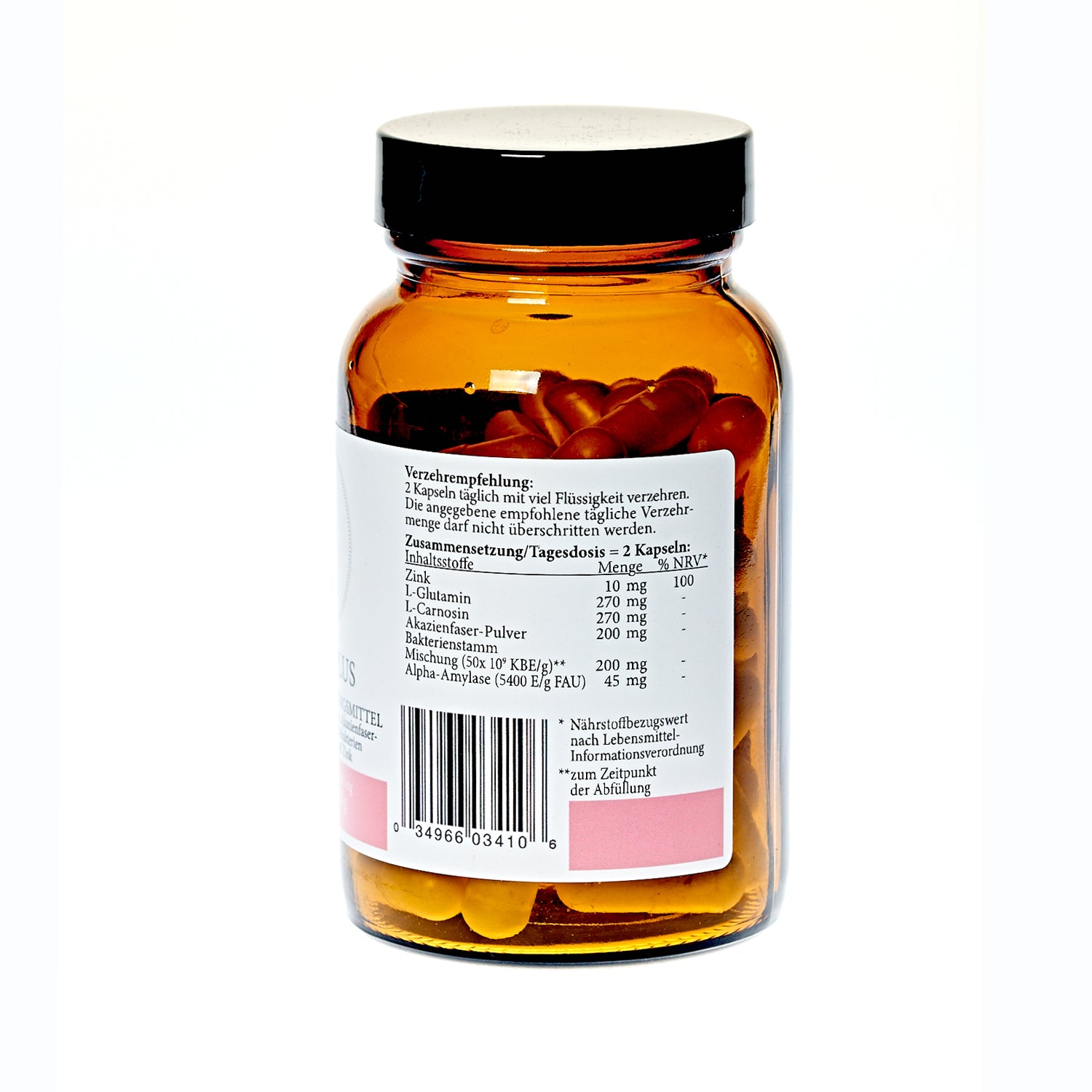
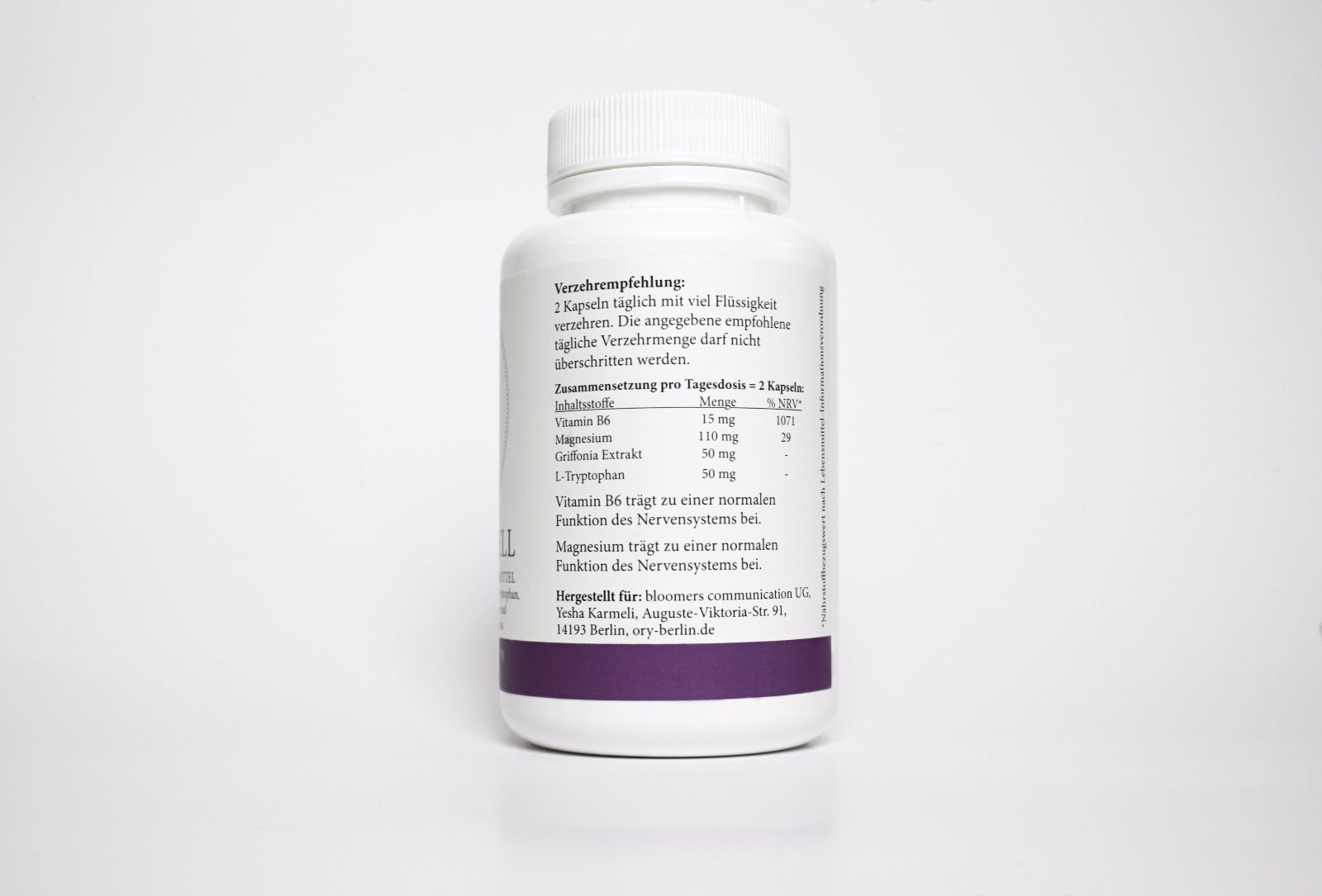
Microbiome Maxi Plus + Leaky Gut + Resorption
More vitality, better nutrition, real health – it all starts in your gut.
Intestinal checkup & microbiome analysis
Your gut is the center of your health. A stable microbiome protects against inflammation, keeps your skin healthy, and supports the production of happiness hormones like serotonin. Fungal infections and silent inflammation, on the other hand, can stifle your vitality. A targeted gut checkup shows where your body needs support. With our partner laboratory, we ensure the highest quality – and provide you with clear, therapeutic recommendations. Start your journey to better health and joy in life now.
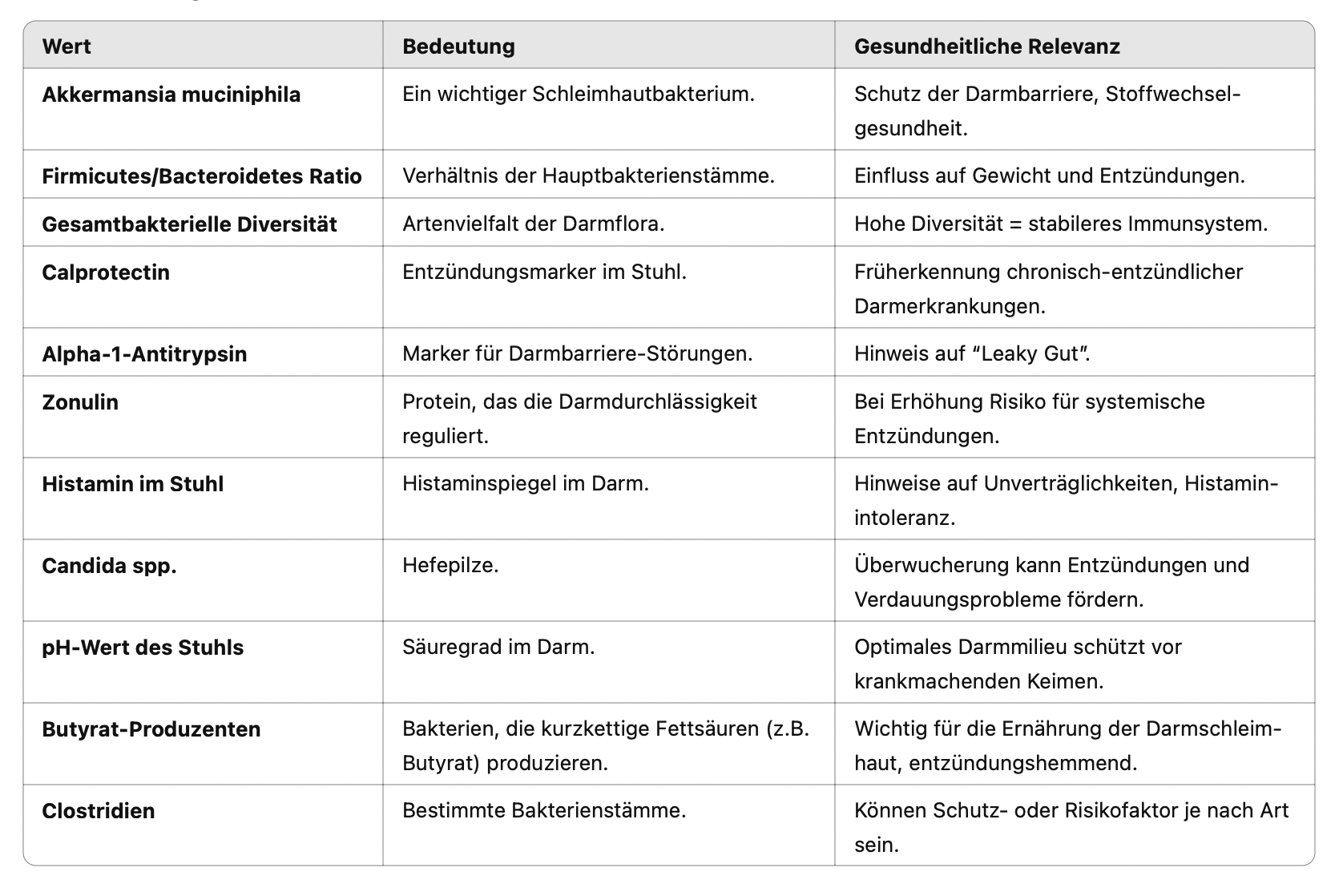
Why are these values important?
- A balanced ratio of good and bad bacteria is crucial for digestion, immune defense and metabolism.
- Chronic inflammation in the intestines often remains asymptomatic for a long time – early detection protects against more serious diseases.
- Histamine breakdown problems can cause irritable bowel syndrome, headaches and skin problems.
- An excess of fungi such as Candida can disrupt the balance of the intestinal flora.
- A leaky gut is associated with autoimmune diseases and allergies.
The microbiome – the totality of intestinal bacteria
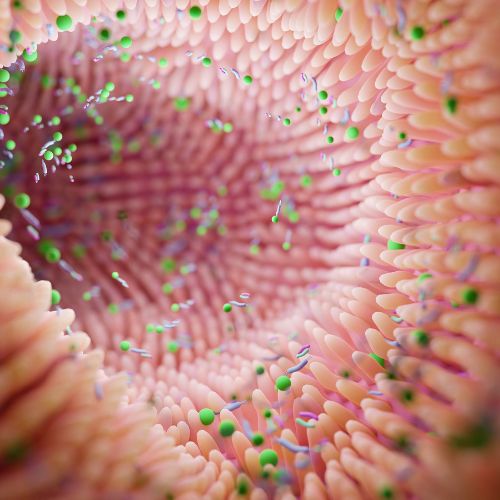
Intestinal bacteria are divided into aerobic (oxygen-dependent) and anaerobic (oxygen-independent) bacteria. Their distribution provides information about where in the intestine certain microorganisms are located and how they relate to our well-being. Aerobic bacteria are found predominantly in the large intestine. These primarily include Escherichia coli and Enterococcus spp.
Colonization of yeasts and molds
Intestinal fungi are usually yeasts of the genus Candida albicans. These yeasts break down carbohydrates from food into carbon dioxide and fusel alcohols . The gas causes bloating, a feeling of fullness, and pain in the intestinal area.

The pH value in the intestine
Acidity (pH) is used to assess the intestinal environment. The detection of an alkaline (basic) stool pH can indicate disturbances in intestinal ecology. It is often the result of excessive amounts of bacterial metabolites from E. coli, enterobacteria, and/or clostridia. Learn more
A modern phenomenon: Leaky Gut
Leaky gut means that the barrier function of the mucous membrane of the small intestine is impaired. As a result, bacteria and toxins from the intestine can enter the bloodstream and promote systemic inflammation. Possible symptoms can include diarrhea, bloating, fatigue, decreased performance, and food allergies and intolerances.

Intestinal reconstruction program
– Step by step to healthy digestion:
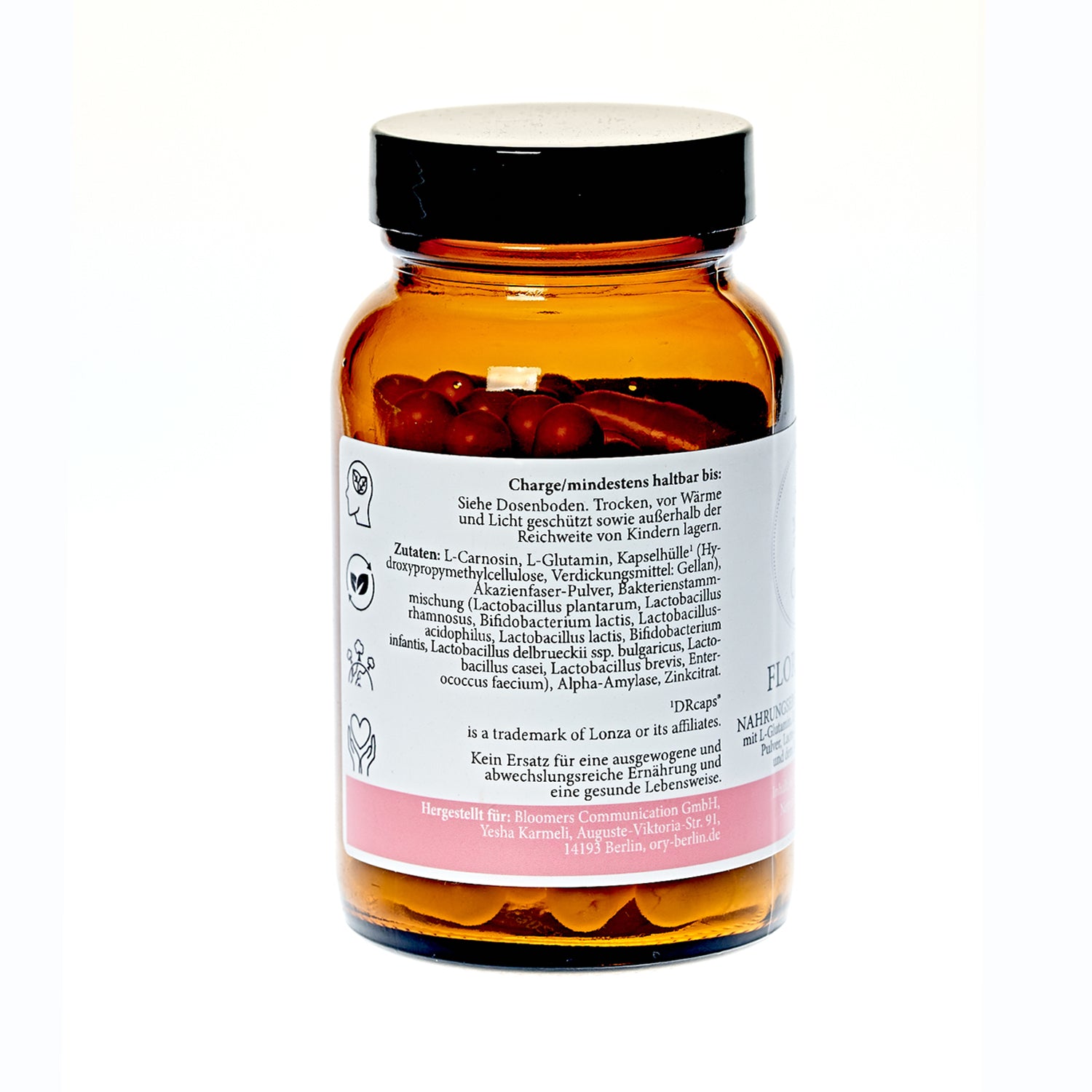
strengthen the microbiome and bring good bacteria back into balance.
support the breakdown of nutrients and relieve the intestines.
stimulate the liver, bile and digestive juices – for an active metabolism.
FAQs
What is a gut microbiome/gut flora?
The gut microbiome/intestinal flora, often simply referred to as the microbiome, encompasses all microorganisms living in the human gut. These microorganisms consist primarily of bacteria, but also include viruses, fungi, and archaea. Here are some important aspects of the gut microbiome:
Composition and function of the intestinal microbiome
Bacteria: Number and diversity: Approximately 100 trillion bacterial cells live in the human gut, making the microbiome one of the largest microbial communities in the body.
Main groups: The most important bacterial phyla in the intestine are Firmicutes, Bacteroidetes, Actinobacteria and Proteobacteria.
Functions of the intestinal microbiome
Digestion and nutrient absorption:
Fermentation: Bacteria ferment indigestible food components (such as fiber) and produce short-chain fatty acids (SCFAs) such as butyrate, acetate, and propionate, which serve as an energy source for the intestinal mucosa and other tissues.
Synthesis of vitamins: Some bacteria in the intestine are able to synthesize vitamins such as vitamin K and some B vitamins.
Immune system: Immune system modulation: The microbiome plays an important role in the development and function of the immune system. It helps defend against pathogens and regulates inflammatory processes.
Barrier function: The microorganisms support the integrity of the intestinal barrier and prevent the penetration of harmful substances.
Metabolism and weight control: Metabolism: The microbiome influences metabolism, including energy production from food and the regulation of body weight.
Hormone production: Some intestinal bacteria produce hormones and neurotransmitters that can influence appetite and metabolism.
Protection against pathogens
Competition: The microbiome competes with pathogenic microorganisms for nutrients and attachment sites in the intestine, making colonization by pathogens more difficult.
Production of antimicrobial substances: Some bacteria produce substances that kill pathogenic germs or inhibit their growth.
Factors that influence the microbiome
Nutrition: High-fiber diet: Promotes the growth of beneficial bacteria that ferment fiber.
Sugar and fat: A diet rich in sugar and fat can lead to dysbiosis (imbalance of microflora).
Taking antibiotics:
Can severely alter the microbiome and deplete beneficial bacteria, leading to temporary or long-term dysbiosis.
Lifestyle and environment:
Stress: Chronic stress can negatively affect the microbiome.
Hygiene: Excessive hygiene and disinfection can reduce exposure to beneficial microbes.
Importance of the microbiome for health
A healthy gut microbiome is crucial for overall well-being. Disruptions in the microbiome are associated with a variety of health problems, including:
Digestive disorders: Such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
Metabolic diseases: Such as obesity and type 2 diabetes.
Mental health: There is evidence that the microbiome influences brain function and mood (gut-brain axis).
Microbiome research is a dynamic field that continues to provide new insights into the complex interactions between microorganisms and human health.
How can you determine whether your intestinal flora is healthy?
There are various methods available to assess the state of the intestinal flora, providing information about the composition and balance of microorganisms in the intestine. One of the most common and informative methods is the stool test. This involves examining the stool sample for various parameters. Below are the most important aspects for assessing intestinal health:
1. Stool test (microbiome analysis)
A comprehensive stool test provides valuable information about the diversity and balance of intestinal bacteria. Typically, the following points are analyzed:
• Bacterial diversity: number and types of microorganisms present
• Dominant bacterial groups: ratio of beneficial to potentially harmful bacteria
• Pathogenic germs: Detection of pathogenic bacteria, viruses or parasites
• Inflammatory markers: Values such as calprotectin, which can indicate inflammatory processes in the intestine
• Digestive residues: Indication of incompletely digested food components
• pH of stool: An important indicator of the intestinal environment
2. Intestinal flora analysis by our specialized laboratories
Specialized microbiome laboratories offer in-depth analyses that go beyond standardized stool tests. They enable precise assessment of microbial composition and provide profound insights into the diversity and balance of the intestinal flora.
How do I know if I have leaky gut?
Leaky gut syndrome can be diagnosed through special laboratory tests. The following markers are particularly informative:
Central markers:
• Zonulin: An increased zonulin value in the stool directly indicates increased permeability of the intestinal mucosa.
• Calprotectin: An inflammatory marker that indicates silent or active inflammation in the intestine.
Further indications of a disrupted intestinal barrier:
• Alpha-1 antitrypsin: May be elevated in cases of inflammatory activity and permeable intestinal wall.
• Histamine in the stool: Can indicate regulatory disorders, inflammation or bacterial imbalances.
Additional tendencies in impaired bowel function:
• Microbiome imbalance: imbalance between beneficial and harmful bacteria
• Clostridial infection: May be associated with inflammation and increased intestinal permeability
• Digestive residues and pH shifts: Indications of impaired digestion and intestinal milieu. Our ORY stool analysis is specifically designed for diagnosing leaky gut syndrome and provides precise values for assessing your intestinal barrier and microbiome balance. Our experts will support you individually through the evaluation and further steps.
What is Akkermansia muciniphila?
Akkermansia muciniphila is a beneficial intestinal bacterium that lives in the large intestine, where it breaks down and renews the protective mucin layer of the intestinal mucosa. It is considered an important aid to intestinal health and is the focus of modern microbiome research.
Why is Akkermansia muciniphila important?
• Strengthens the intestinal barrier: Supports the renewal of the protective mucous membrane and prevents the penetration of harmful substances.
• Anti-inflammatory: Promotes anti-inflammatory processes in the intestine.
• Good for metabolism: Associated with better insulin sensitivity and healthier body weight.
• Immunoregulatory: Contributes to a balanced immune response.
How can Akkermansia be promoted?
• Prebiotics: Fiber such as acacia fiber or oligofructose
• Polyphenols: E.g. from berries, green tea or red wine
• Healthy lifestyle: balanced diet and regular exercise
• Future option: Direct intake as a probiotic is currently being researched
Which tests should be done for intestinal fungus?
To reliably diagnose intestinal fungus (candidiasis), specific tests are usually performed, particularly a stool sample. Here are the key steps and methods used to diagnose intestinal fungus:
Stool examination
Stool culture: Stool is examined in the laboratory to identify fungi such as Candida spp. This is done by creating a culture in which the growth of fungi is promoted under special conditions.
Microscopic examination: The culture is examined under a microscope to identify fungal spores and hyphae.
Quantitative analysis: In addition to the mere presence, the amount of Candida fungi is often determined to assess whether there is a pathogenic colonization.
How do I know if I have a fungus in my body?
Fungal infections in the body can cause various symptoms, depending on where they occur. A targeted stool test is a useful and non-invasive method for detecting possible intestinal fungal infections (e.g., Candida) early.
Why is stool diagnostics useful?
A stool analysis can provide evidence of fungal infection in the gut—often a starting point for further problems in the body. Overgrowth of yeasts such as Candida albicans can disrupt the microbiome and promote inflammation.
Typical symptoms of intestinal fungus:
• Bloating, abdominal pain
• Diarrhea or constipation
• Sugar cravings
• Fatigue, concentration problems
In addition to fungi, stool diagnostics also check other relevant parameters such as microbiome balance, inflammatory markers (e.g. calprotectin) and digestive residues – a holistic approach for targeted therapy.
Other possible fungal infections in the body
1. Skin fungus:
Itching, redness, scaling – often on feet, hands, groin
2. Nail fungus:
Thickened, discolored, brittle nails (usually toes)
3. Oral thrush:
White deposits, burning, difficulty swallowing
4. Vaginal yeast infection:
Itching, burning, whitish discharge, pain when urinating. Conclusion:
A stool examination is a useful first step to determine whether there is a fungal infection in the intestine – especially in cases of unclear symptoms or recurring infections.
Our ORY stool analysis is specifically designed to provide valuable insights into intestinal and fungal health.
Histamine in the intestine – what does that mean?
In a healthy gut, histamine ingested with food or produced by bacteria is broken down by DAO. If this function is disrupted, histamine buildup occurs, which can lead to symptoms such as:
• Flatulence, diarrhea, abdominal pain
• Heartburn, nausea, cramps
• Cravings for sweets, feeling of fullness
An increased histamine level in the stool indicates impaired histamine utilization and a possible microbial imbalance – especially when histamine is released simultaneously by unfavorable intestinal bacteria.
Causes of histamine intolerance
• DAO deficiency (genetic or acquired)
• Microbiome imbalance with histamine-producing germs
• Histamine-rich diet (e.g. mature cheese, alcohol)
Our ORY stool analysis specifically measures histamine in the stool as well as important accompanying markers such as DAO activity, microbial balance, inflammatory values (e.g. calprotectin) and dysbiosis tendencies.
This gives us a clear picture of the condition of your intestines and possible causes of your symptoms.
What helps with histamine intolerance?
• Low-histamine diet: Avoid foods that are rich in histamine or release histamine
• DAO preparations: Enzyme supplement to support histamine breakdown before eating
• Probiotics and prebiotics: Building a healthy intestinal flora
• Fiber & digestive enzymes: Promote intestinal health and better nutrient utilization
Histamine intolerance (HIT) occurs when the body cannot adequately break down excess histamine—usually due to reduced activity of the enzyme diamine oxidase (DAO) in the intestine. Histamine is a natural messenger substance, but when present in excess, it plays a role in inflammation, digestive problems, and food intolerances.
Histamine intolerance often originates in the intestines. A targeted stool analysis with histamine measurement—such as the ORY analysis—provides important clues to the causes and enables individualized treatment. Our experts will be happy to advise you.