
The importance of the microbiome – especially with regard to the first microbial colonization in newborns
Modern research repeatedly shows that our health is influenced not only by external factors such as diet and environment, but also significantly by the microbiome that populates our bodies. The timing and manner in which this complex ecosystem is first established in life play a crucial role. Birth—as the first and most intensive contact between mother and child—is a key focus here. While a vaginal delivery involves a natural transmission of microorganisms, the colonization during a cesarean section differs significantly. These differences have not only immediate but also long-term health consequences.
The microbiome: importance and initial colonization
The microbiome encompasses all microorganisms—bacteria, viruses, fungi, and other microbes—that live in and on our bodies. These communities fulfill important functions:
-
Training the immune system: A diverse microbial colonization helps to “train” the immune system early on so that it learns to distinguish between harmless and potentially harmful antigens.
-
Metabolism and nutrient absorption: A well-established microbiome supports metabolism and contributes to the production of vital substances.
-
Protection against pathogens: The microbes compete with pathogenic organisms and thus prevent their overgrowth.
The first colonization of the newborn represents a crucial moment. This depends on the transfer of the maternal microbiota – a process that varies greatly depending on the mode of birth.
Different microbiome colonization: Vaginal vs. Caesarean section
Vaginally delivered children
Studies, most notably the study by Dominguez-Bello et al. (2010, PNAS) , have shown that newborns born vaginally primarily receive microorganisms from the mother's birth canal. These pathogens include, for example, Lactobacillus and Bifidobacterium , which are typically found in the vagina. These bacteria are not only essential for a diverse microbiome structure but also contribute to optimally conditioning the immune system from the start.
Children born by cesarean section
In contrast, babies born by cesarean section primarily receive microorganisms from the mother's skin and the surrounding environment. These differences manifest themselves in the following aspects:
-
Reduced diversity: Microbial diversity in the first months of life is often reduced due to the lack of transmission of the vaginal microbiota – a key factor for early immune development.
-
Altered composition: Instead of the typical anaerobic bacteria from the birth canal, bacteria that are more commonly associated with the skin or the hospital environment dominate.
The meta-analysis by Bager et al. (2008, Clinical & Experimental Allergy) concludes that infants born by cesarean section have an approximately 20–30% increased risk of suffering from immune-mediated diseases such as asthma, allergies, and atopic diseases. Altered microbial colonization represents a key mechanism that can impair the normal development of the immune system.
Long-term health effects
The consequences of the initial microbial colonization affect health for years:
-
Asthma and respiratory diseases: An insufficiently trained immune system can impair the ability to distinguish between harmless and harmful antigens. Studies show that the risk of childhood asthma is significantly increased in children born by cesarean section.
-
Allergies and atopic diseases: A diverse and stable microbiome structure has a protective effect. However, a deficiency of important microorganisms can promote the development of allergies.
-
Metabolic disorders and chronic diseases: In addition to the direct influence on the immune system, microbial colonization also influences metabolism and thus the risk of later chronic diseases.
These findings underpin the basic idea of the microbiome concept: not the blind elimination of germs, but the targeted promotion of a balanced, natural microbiome community is crucial for long-term health.
Caesarean section as a phenomenon of our time
Increasing number of caesarean sections
In recent decades, there has been a significant increase in cesarean sections worldwide. Several factors play a role:
-
Medical indications: In cases of risky situations or complications during pregnancy and childbirth, a cesarean section is often the safer alternative.
-
Planned cesarean sections: In addition to purely medical reasons, more and more women are consciously choosing to have a cesarean section. This can be due to various personal and psychosocial reasons.
Psychosocial dimensions of birth
Birth is far more than a medical act—it is a profound experience that profoundly shapes the mother's identity and self-confidence. Several studies have shown that:
-
The experience of natural birth is closely linked to the development of an intensive mother-child bond.
-
Oxytocin production , which is stimulated during vaginal births, plays an important role in postnatal healing and emotional bonding.
-
The experience of birth itself – as a ritual of transition – influences the woman’s self-confidence and psychological well-being.
These aspects shed light on the cultural problem that in our modern society there is often a “bacteria aversion”, while at the same time the natural processes and the interaction between mother and child are underestimated.
Cultural Perspectives: Bacteria as an Essential Part of Our Being
Many cultures have an ambivalent relationship with microorganisms. On the one hand, they are feared as pathogens, but on the other, they are essential to our health. The following aspects illustrate this dichotomy:
-
Stigmatization vs. Integration: While hygiene and disinfection are highly valued in modern society, it is often overlooked that excessive germ reduction can lead to a one-sided microbiome structure.
-
Bacteria as constant companions: Every touch, every kiss, and every hug leads to an exchange of microbes. These interactions are not random, but contribute to the constant refreshment and diversification of our microbiome.
-
Reorientation of the health concept: The knowledge of the importance of a diverse microbiome suggests that we should fundamentally rethink our attitude towards bacteria. The goal must be to promote a healthy and stable microbial ecosystem rather than destroying it through excessive disinfection.

Bowel check-up for children and adolescents
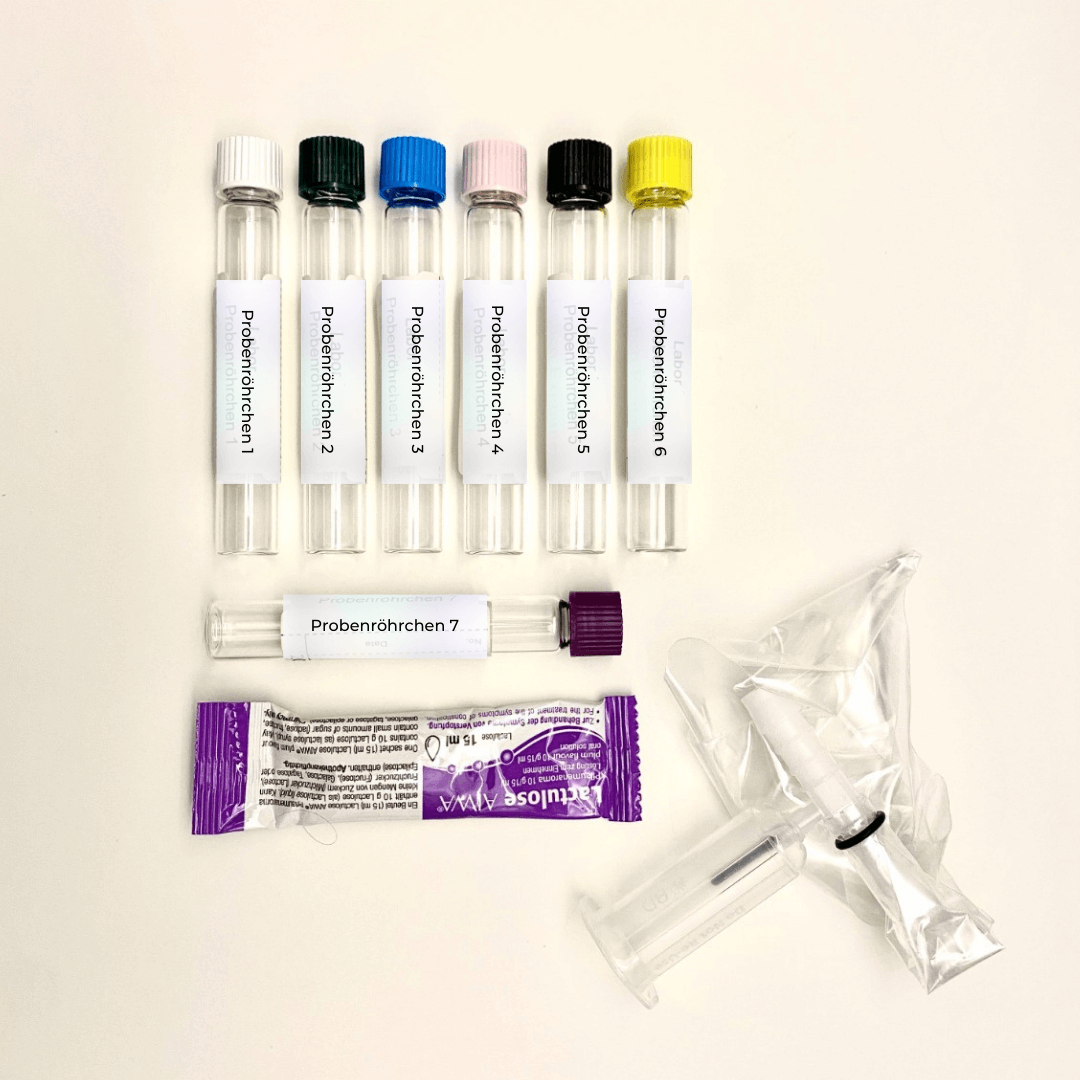
✓ Basic profile intestine | Microbiome & Leaky Gut & Histamine & Akkermansia + F.prausni
Practical implications and future perspectives
The findings from the studies have direct implications for clinical practice and future research:
-
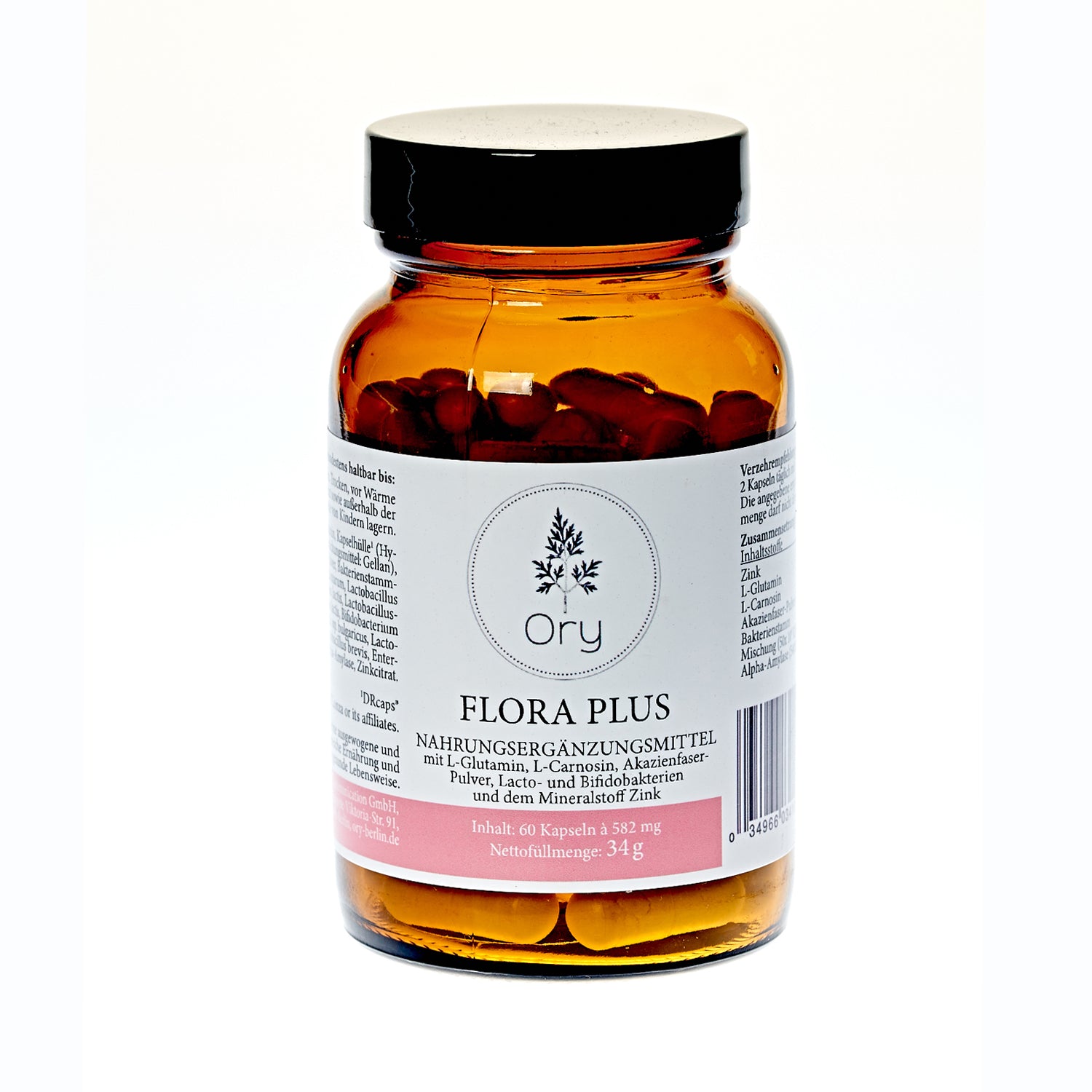
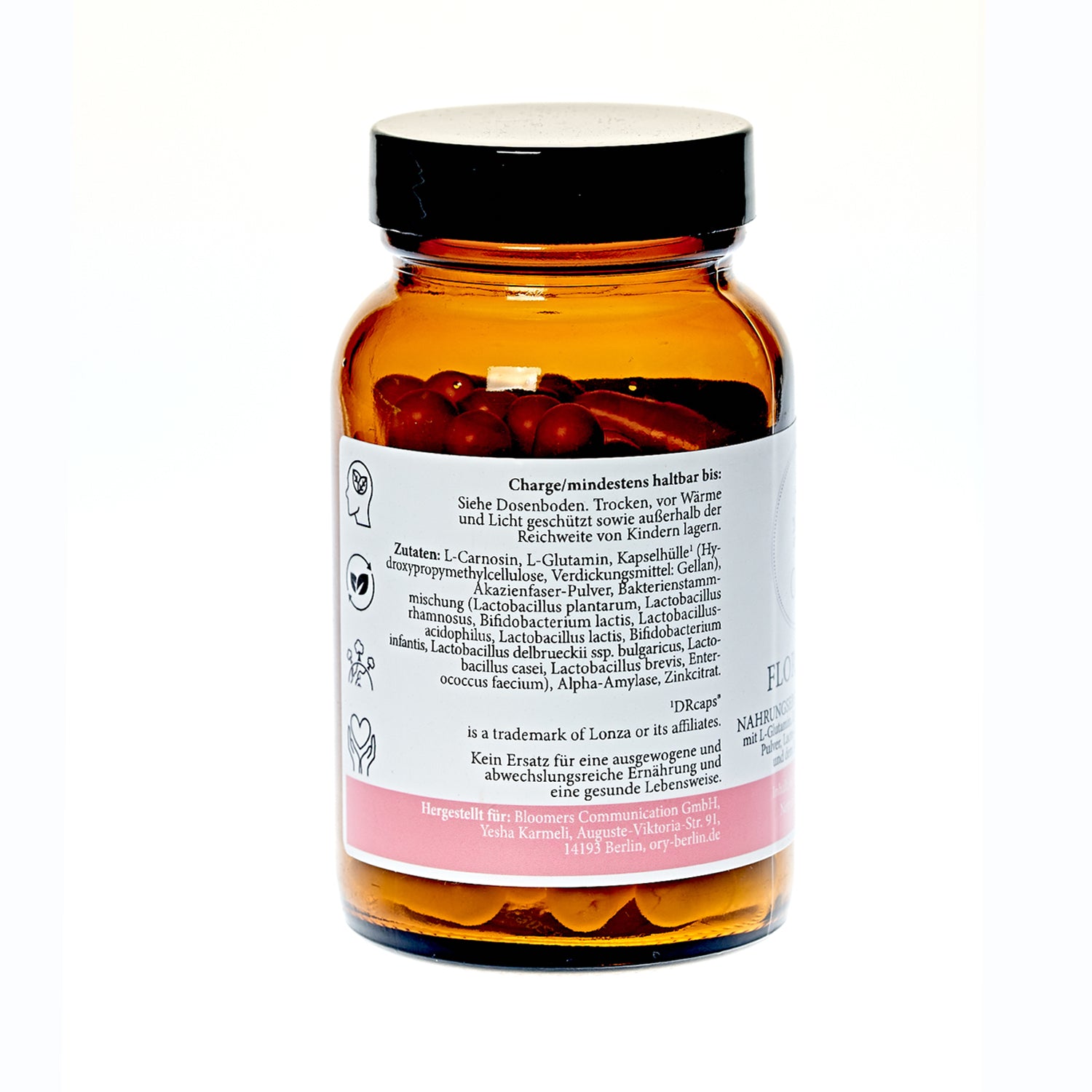
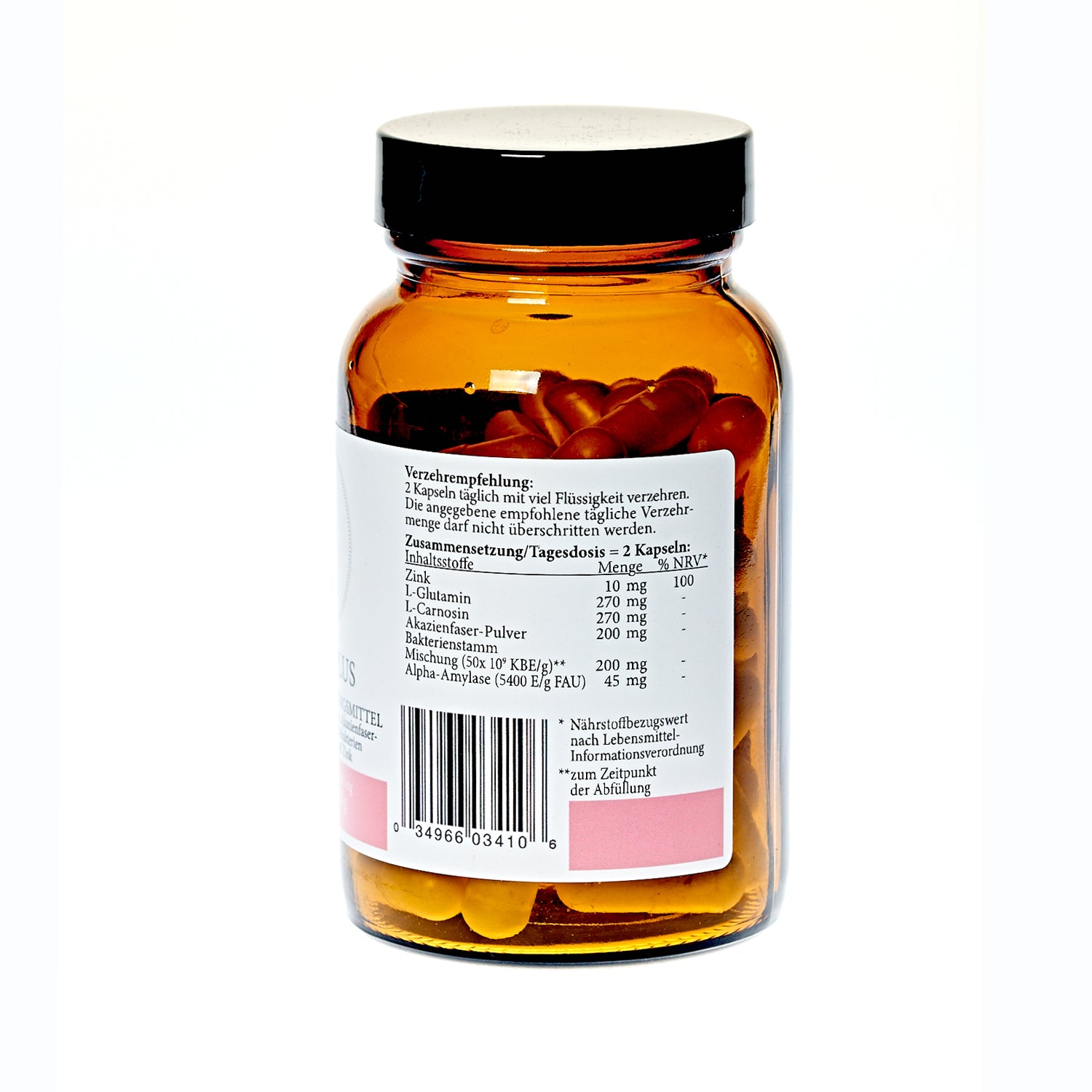
Targeted microbiome remediation: Especially in cases of cesarean section, the targeted promotion of natural colonization – for example through probiotic applications or the so-called vaginal seeding method – could help to compensate for the initial microbiome deficiency.
-
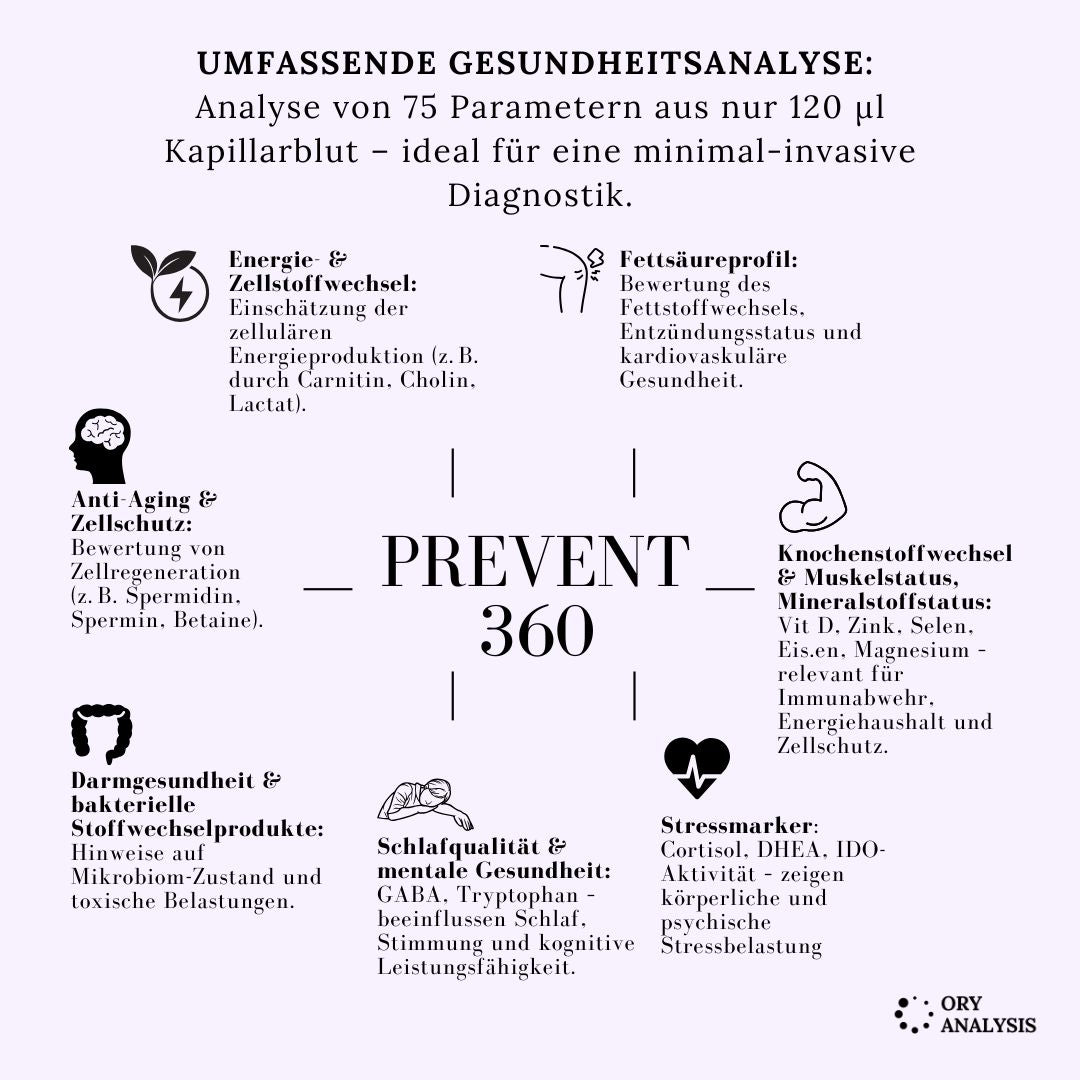
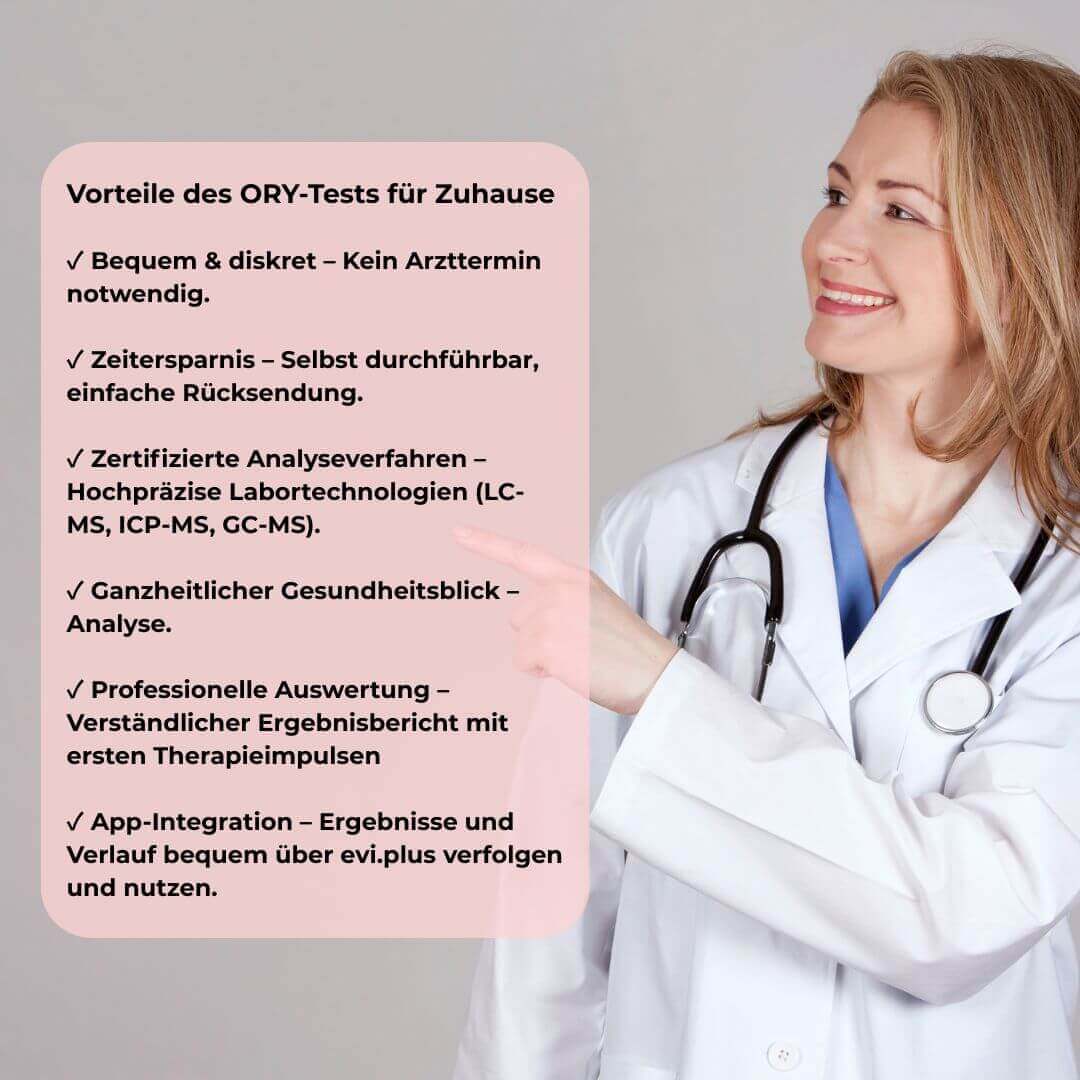
Microbiome testing: Regular analysis of the microbiome could serve as a diagnostic tool in the future to detect imbalances early and take targeted countermeasures.
-
Education and prevention: A comprehensive understanding of the role of the microbiome should be incorporated into counseling for expectant parents. The benefits of natural childbirth, not only from a medical but also from a psychosocial perspective, should be emphasized in the context of the child's health.
-
Interdisciplinary research: The interface between microbiome research, psychology, and obstetrics offers an exciting field to further explore the long-term effects of birth mode on child development.
The way in which a newborn's microbiome establishes itself has far-reaching consequences for their future health.
Numerous studies show that children born vaginally benefit from a natural and diverse transfer of vital microorganisms, while cesarean births are associated with altered microbial colonization and an increased risk of diseases such as asthma, allergies and atopic diseases.
At the same time, it becomes clear that the trend toward increased and even voluntary caesarean sections is a phenomenon of our time—a phenomenon that encompasses not only medical but also psychosocial and cultural dimensions. Birth as an experience that strengthens the mother-child bond and supports postnatal healing takes a back seat when natural processes are artificially circumvented.
It therefore seems all the more important to place the concept of the microbiome at the center of healthcare: The goal is not to eliminate bacteria, but to promote a stable and diverse microbial environment that trains the immune system, optimizes metabolism, and provides long-term protection against chronic diseases. Future approaches in obstetrics and neonatal care should therefore be integrated—including targeted microbial interventions and increased education about the importance of natural microbiome transmission.
Overall, a deeper understanding of the role of the microbiome not only opens up new perspectives for the prevention and treatment of numerous diseases, but also challenges us to re-evaluate our cultural relationship with microbes and bring it into a health-promoting balance.






























Share:
Chromium – friend or foe?
Dementia and nutrients – Mitochondrial dysfunction & brain activity